Introduction
Urinalysis is the cornerstone of veterinary diagnostics. This simple, non-invasive test provides a wealth of information about kidney function, metabolic disorders, infections, and systemic diseases. Complete urinalysis consists of three integrated (physical, chemical & microscopic examination) components that work together to provide a comprehensive picture of your animal’s health. When performed carefully, urinalysis can reveal early signs of disease, help in monitoring treatment, and guide further laboratory investigations.
Sample Handling
Analyze within 30 minutes of collection. If delayed, refrigerate at 4°C (maximum 6-12 hours). Room temperature storage causes:
- Bacterial proliferation
- Crystal dissolution/formation
- Cellular degradation
- pH elevation (bacterial urease activity)
- Glucose consumption
The Three Pillars of Urinalysis:
- Physical Analysis – Color, clarity, and specific gravity
- Chemical Analysis – Dipstick testing for multiple parameters
- Microscopic Analysis – Sediment examination for cells, casts, crystals, and organisms
PART 1: PHYSICAL ANALYSIS
Volume
Normal output: Daily urine output depends on species, age, hydration, and diet
- Dog: 20–40 ml/kg/day
- Cat: 20–40 ml/kg/day
- Horse: 3–18 L/day
- Cattle: 5–15 L/day
- Sheep/goat: 0.5–2.5 L/day
Clinical significance:
- Polyuria (>50 mL/kg/day): diabetes mellitus, chronic kidney disease, hyperadrenocorticism, hyperthyroidism (cats), psychogenic polydipsia
- Oliguria (<1 mL/kg/hr): dehydration, acute kidney injury, urethral obstruction, shock
- Anuria: complete urinary obstruction, bilateral renal failure, ruptured bladder
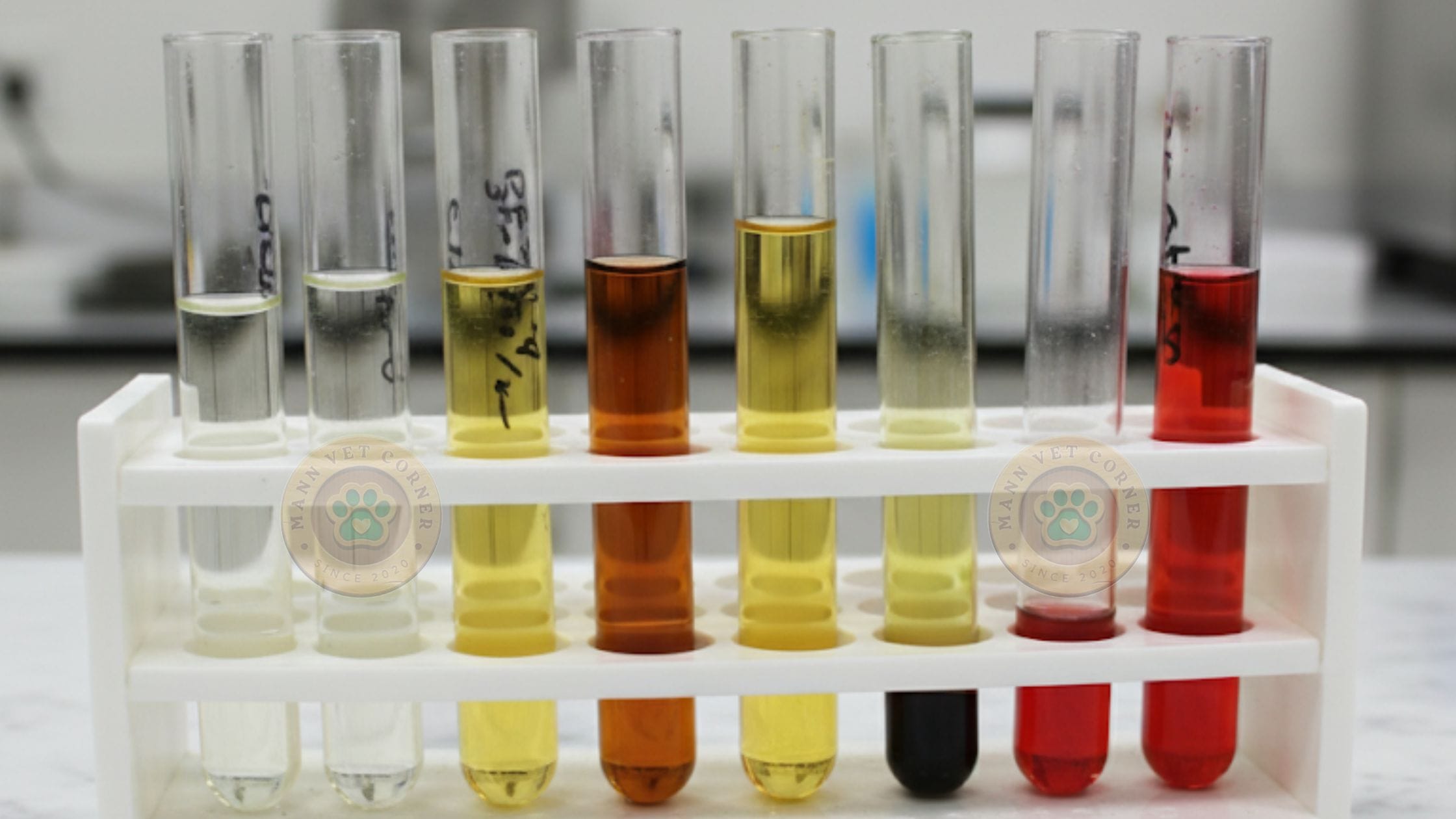
Color
Normal: Pale yellow to amber (urochrome pigment concentration-dependent)
Normal urine color varies by species:
- Dogs and cats: light yellow to amber.
- Cattle and horses: yellow to dark amber.
- Horse urine may appear cloudy due to calcium carbonate crystals (normal).
- Red/brown: Hematuria (intact RBCs), hemoglobinuria (intravascular hemolysis), myoglobinuria (rhabdomyolysis)
- Orange: Concentrated urine, bilirubin, rifampin administration
- Yellow-brown/green: Bilirubinuria (hepatobiliary disease)
- Colorless: Extreme dilution (specific gravity <1.008)
- White/cloudy: Pyuria, crystalluria, lipiduria
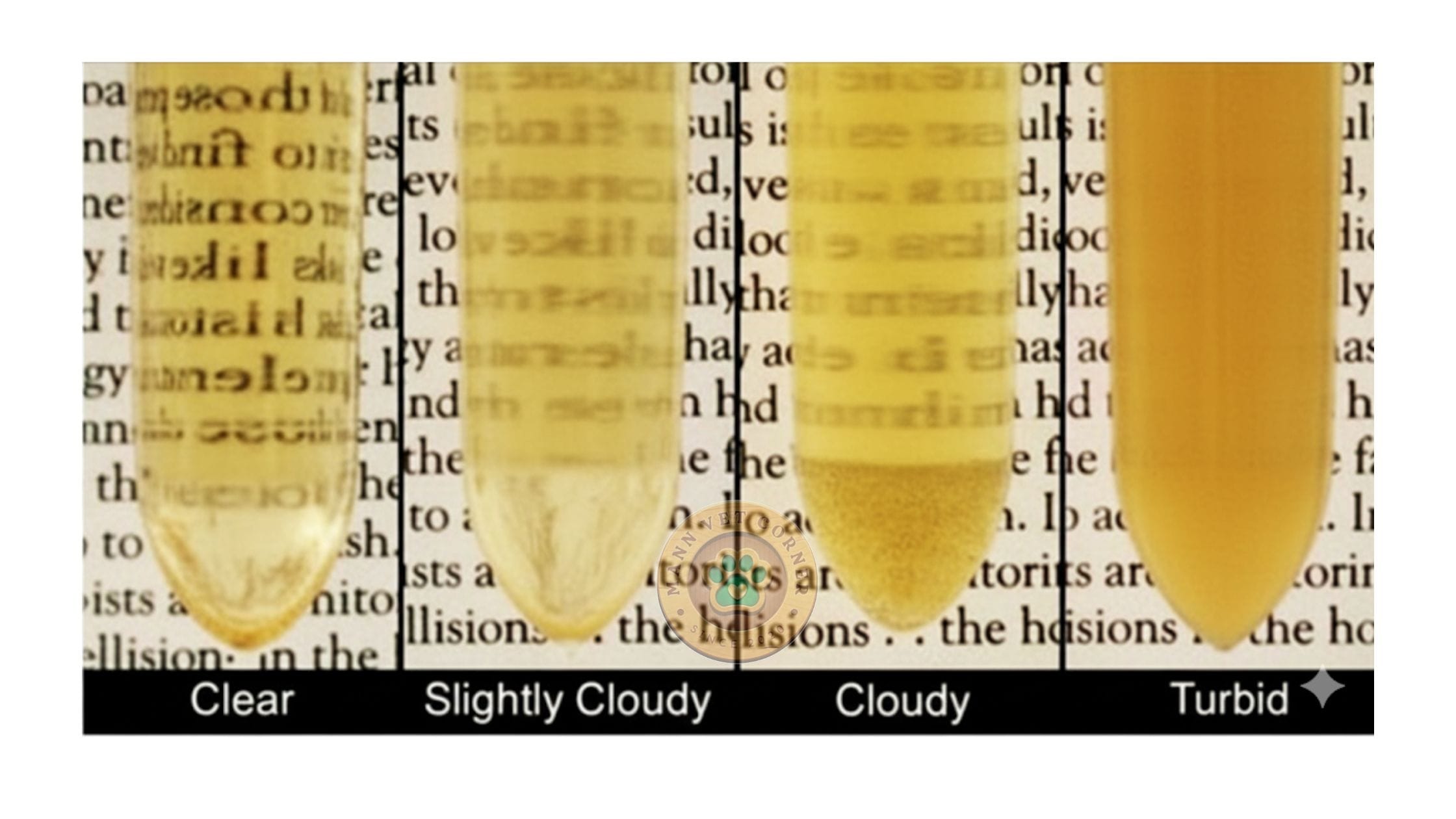
Turbidity
Clear: Normal fresh urine
- Small animals (dogs, cats, cattle): urine should be clear.
- Horses, rabbits, guinea pigs: urine may normally be cloudy or milky due to calcium carbonate crystals and mucus.
- Pathological turbidity: pus, cells, bacteria, crystals, or fat droplets.
Cloudy: Cells (WBCs, RBCs, epithelial), bacteria, crystals, mucus, spermatozoa, lipids
Refrigerated samples may develop artifactual turbidity from calcium carbonate (herbivores) or phosphate crystal precipitation.
Odor
Normal: Faint aromatic Ammonia: Bacterial urease conversion of urea (UTI, old sample)
Sweet/fruity: Ketonuria (diabetic ketoacidosis, starvation) Putrid: Severe bacterial infection, necrotic tissue
Specific Gravity (USG)
Measures urine concentration relative to distilled water; reflects renal tubular concentrating ability.
Measurement: Refractometry (preferred; temperature-compensated) or urinometer
Reference ranges:
- Dogs: 1.015-1.045
- Cats: 1.035-1.060
- Cattle: 1.025-1.045
- Horses: 1.025-1.050
Clinical interpretation:
- Isosthenuric (1.008-1.012): Inappropriate concentration; chronic kidney disease, hypoadrenocorticism, hepatic failure, diabetes insipidus
- Hyposthenuric (<1.008): Active dilution; psychogenic polydipsia, central diabetes insipidus, early renal disease
- Adequately concentrated (>1.030 dogs; >1.035 cats): Normal renal function with appropriate ADH response
- Inappropriately concentrated: Dehydration with USG <1.030 suggests renal dysfunction
The Golden Rule
- Dehydrated + High USG = Normal kidneys
- Dehydrated + Low/Isosthenuric USG = Kidney disease
Note: Glucosuria, proteinuria, and contrast agents falsely elevate USG.
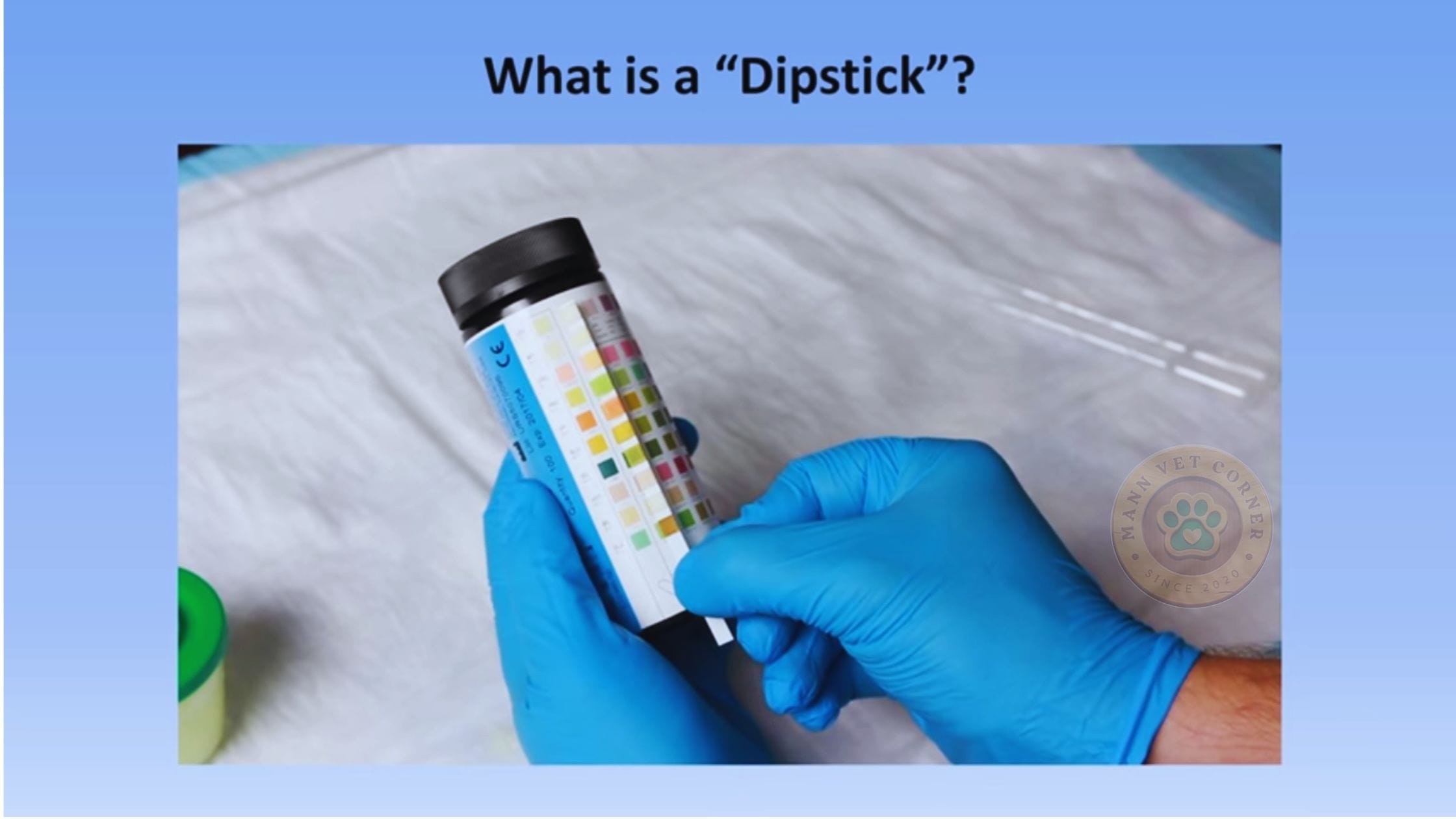
PART 2: CHEMICAL ANALYSIS
Urine Dipstick Testing
Chemical analysis uses reagent strips (dipsticks) to detect multiple parameters simultaneously. Results are semi-quantitative and must be interpreted with physical and microscopic findings.
Timing: Perform chemical analysis immediately after physical examination.
Proper Dipstick Technique
- Check expiration date – discard outdated strips
- Mix urine sample thoroughly
- Dip strip briefly (1 second) – completely immerse pads
- Remove excess – tap edge against container
- Hold horizontally – prevents pad cross-contamination
- Time readings precisely – each pad has specific timing (30-120 seconds)
- Read in good lighting – compare to color chart on bottle
- Record immediately
Important: Do not touch test pads. Keep strips in original container with desiccant.
Chemical Parameters
1. pH
What It Measures: Acid-base balance of urine
Normal ranges:
- Carnivores (dogs, cats): 5.5-7.0 (slightly acidic)
- Herbivores (horses, cattle, rabbits): 7.0-9.0 (alkaline)
Clinical significance:
- Acidic (<6.0): High-protein diet, acidosis (diabetic, lactic), paradoxical aciduria (hypokalemia), cranberry supplements, acidifying drugs
- Alkaline (>7.5): UTI with urease-producing bacteria (Staphylococcus, Proteus), post-prandial alkaline tide (herbivores), alkalemia, distal renal tubular acidosis
Crystal formation:
- Struvite: Favored at pH >7.0
- Calcium oxalate: Forms at pH <6.5
- Urate: Precipitates at pH <6.0
2. PROTEIN (Normal: Negative to Trace)
What It Measures: Protein in urine (primarily albumin). Results: Negative, Trace, 1+, 2+, 3+, 4+
Normal: Trace amounts (<30 mg/dL); dipstick negative to trace
Method: Colorimetric; most sensitive to albumin (may miss Bence Jones proteins)
Interpretation: Quantify with urine protein:creatinine ratio (UPC)
- Normal: <0.2 (dogs), <0.4 (cats)
- Borderline: 0.2-0.5 (dogs), 0.4-0.5 (cats)
- Proteinuric: >0.5 (dogs), >0.5 (cats)
Causes:
- Pre-renal: Hemoglobinuria, myoglobinuria, Bence Jones proteins (multiple myeloma)
- Renal: Glomerulonephritis, amyloidosis, glomerulosclerosis, pyelonephritis, tubular damage
- Post-renal: UTI, urolithiasis, neoplasia, genital contamination
False positives: Alkaline urine (pH >8.0), quaternary ammonium disinfectants, concentrated urine
3. GLUCOSE (Normal: Negative)
What It Measures: Glucose in urine. Normal: Absent in urine
Renal threshold:
- Dogs: ~180 mg/dL blood glucose
- Cats: ~280 mg/dL blood glucose
Mechanism: Filtered glucose exceeds proximal tubular reabsorption capacity
Causes:
- Hyperglycemic: Diabetes mellitus, stress hyperglycemia (cats), hyperadrenocorticism, acute pancreatitis, IV glucose administration
- Normoglycemic: Fanconi syndrome (primary renal glucosuria), proximal tubular damage (aminoglycosides, heavy metals)
False negatives: Ascorbic acid interference, bacterial consumption (delayed analysis)
Clinical Significance:
- With polyuria/polydipsia and high USG → suspect diabetes mellitus
- Always correlate with blood glucose
- Persistent glucosuria → check for concurrent ketonuria (diabetic ketoacidosis)
4. KETONES (Normal: Negative)
What It Measures: Acetoacetic acid and acetone (not beta-hydroxybutyrate). Normal: Absent
Detection: Acetoacetate and acetone (not β-hydroxybutyrate, the predominant ketone)
Causes:
- Pathologic: Diabetic ketoacidosis (most common), starvation ketosis, pregnancy toxemia (ewes, does), bovine ketosis
- Physiologic: Prolonged fasting, high-fat/low-carbohydrate diet, prolonged exercise
Clinical context: Always assess concurrent glucose, pH, and clinical signs
Clinical Significance:
- Ketones + glucose = diabetic ketoacidosis (DKA)
- Ketones without glucose = starvation ketosis or dietary
- DKA requires immediate emergency treatment
5. BLOOD (Normal: Negative)
What It Measures: Intact RBCs, free hemoglobin, or myoglobin
Dipstick reaction: Detects heme pigment (hemoglobin, myoglobin, intact RBCs)
Differentiation:
- Hematuria: RBCs visible on microscopy; red/pink urine with sediment
- Hemoglobinuria: Supernatant remains red after centrifugation; no/rare RBCs on microscopy; associated with hemolysis (pink-red plasma)
- Myoglobinuria: Supernatant red; no RBCs; normal plasma color; elevated CK; history of rhabdomyolysis
Hematuria causes:
- Lower urinary tract: Cystitis, urolithiasis, neoplasia (transitional cell carcinoma), trauma, coagulopathy, idiopathic renal hematuria
- Upper urinary tract: Pyelonephritis, renal infarction, nephrolithiasis, renal neoplasia
Hemoglobinuria causes: IMHA, Babesia, onion/garlic toxicity, zinc toxicosis, hypophosphatemia, transfusion reaction
Myoglobinuria causes: Exertional rhabdomyolysis (horses), malignant hyperthermia, seizures, trauma/crush injury, electrocution
Confirmation: Microscopic examination to differentiate hematuria from hemoglobinuria/myoglobinuria
6. BILIRUBIN (Normal: Negative in cats, trace in dogs)
What It Measures: Conjugated bilirubin in urine.
Normal:
- Dogs: Negative to trace (1+) acceptable, especially concentrated urine; low renal threshold
- Cats: Always abnormal; high renal threshold
- Large animals: Generally absent
Conjugated bilirubin (water-soluble) appears in urine before serum hyperbilirubinemia is detectable.
Causes:
- Hemolytic disease: Immune-mediated hemolytic anemia, Babesia, zinc toxicosis (less common than hepatic)
- Hepatobiliary disease: Hepatitis, cholestasis, cirrhosis, neoplasia, cholangiohepatitis (cats)
- Post-hepatic obstruction: Cholelithiasis, pancreatitis, bile duct neoplasia
Clinical approach: Always evaluate with liver enzymes, complete blood count, and imaging
Clinical Significance:
- Often appears BEFORE serum bilirubin elevates or jaundice visible
- Any bilirubinuria in cats warrants investigation
- Correlate with liver enzymes and bile acids
7. LEUKOCYTES (Variable reliability in veterinary medicine)
What It Measures: Esterase from WBCs
Limitations:
- Designed for human urine
- Less reliable in animals
- Microscopic examination is superior for detecting pyuria
Detects granulocytic esterase activity. High false-negative rate in animals. Always rely on microscopic examination for WBC quantification.
Best Practice: Do not rely on dipstick alone; always perform microscopic examination
9. NITRITE (Limited use in veterinary medicine)
What It Measures: Bacterial conversion of nitrate to nitrite
Why Unreliable in Animals:
- Requires nitrate in diet (carnivores have low nitrate)
- Requires 4+ hours of bacterial incubation in bladder
- Many veterinary pathogens don’t produce nitrite
Detects bacterial conversion of dietary nitrate to nitrite. Many veterinary pathogens lack nitrate reductase. High false-negative rate. Bacterial culture remains gold standard for UTI diagnosis.
Best Practice: Culture urine if infection suspected; do not rely on nitrite test.
PART 3: MICROSCOPIC ANALYSIS
Urine Sediment Examination
Microscopic examination is the most detailed component of urinalysis, revealing cells, casts, crystals, bacteria, and parasites invisible to the naked eye.
Sediment Preparation
Standard Method:
- Use 5-10 mL fresh urine (ideally <30 minutes old)
- Centrifuge at 1500 rpm for 5 minutes
- Pour off supernatant leaving 0.5 mL with sediment
- Resuspend sediment by gentle tapping
- Place drop on slide with coverslip
- Examine systematically
Alternative: Commercial standardized systems (e.g., Kova system) for consistency
Microscopic Examination Technique
Low Power (10x objective):
- Scan entire slide
- Identify casts (low cellularity needed)
- Assess overall cell density
High Power (40x objective):
- Identify and count cells
- Examine crystals
- Identify bacteria
- Report as cells/organisms per high power field (HPF)
Microscopic Components
1. RED BLOOD CELLS (RBCs)
Normal: 0-5 per HPF
Appearance: Small, round, pale, non-nucleated discs (7-8 µm)
Increased RBCs (Hematuria) Causes:
- Urinary tract infection
- Urolithiasis (bladder/kidney stones)
- Trauma
- Tumors (transitional cell carcinoma, renal carcinoma)
- Coagulopathy (thrombocytopenia, rodenticide toxicity)
- Infarction
- Idiopathic cystitis (especially cats)
- Cyclophosphamide-induced cystitis
- Renal parasites
Clinical Correlation:
- Correlate with dipstick blood reaction
- If dipstick positive but no RBCs on sediment → hemoglobinuria or myoglobinuria
2. WHITE BLOOD CELLS (WBCs)
Normal: 0-5 per HPF (dogs/cats)
Appearance: Larger than RBCs, granular, nucleated (10-12 µm)
Increased WBCs (Pyuria) Causes:
Infectious
- Bacterial cystitis (most common)
- Pyelonephritis (kidney infection)
- Prostatitis
- Urethritis
- Vaginitis/balanitis (contamination)
Non-Infectious Inflammation
- Urolithiasis
- Neoplasia
- Idiopathic cystitis
- Catheter trauma
- Chemical irritation
Clinical Significance:
- Pyuria + bacteriuria + clinical signs = UTI (culture recommended)
- Pyuria without bacteriuria → consider fungal infection, early UTI, or sterile inflammation
- Sterile pyuria (no bacteria on culture) → rule out fungal, mycoplasma, or neoplasia
3. EPITHELIAL CELLS
Types:
Squamous Epithelial Cells
- Large, flat, irregular, small central nucleus
- From urethra, vagina, prepuce
- Significance: Indicate sample contamination (free-catch)
- Large numbers reduce diagnostic value
Transitional Epithelial Cells
- Moderate size, round to caudate (tail-like), larger nucleus
- From bladder, ureters, renal pelvis
- Significance: Normal in small numbers
- Increased with inflammation, catheterization, neoplasia
- Clusters with atypia → suspect transitional cell carcinoma
Renal Epithelial Cells
- Smaller, round, large nucleus-to-cytoplasm ratio
- From renal tubules
- Significance: Tubular damage, necrosis, acute kidney injury
- Uncommon; highly significant when present
Caudate Cells
- Transitional cells with characteristic tail
- Normal in cats (up to 15%)
- Not pathological
4. CASTS
What Are Casts? Cylindrical protein structures formed in renal tubules. Their presence indicates renal (kidney) origin of disease.
Tamm-Horsfall protein matrix traps cells/debris, creating casts that wash into urine.
Types and Significance:
Hyaline Casts
- Transparent, colorless, low contrast
- Normal: 0-2 per LPF (low power field)
- Significance: Minimally significant; can occur with fever, exercise, dehydration
Granular Casts
- Contain granules (degenerated cells)
- Fine granular: Early degeneration
- Coarse granular: Advanced degeneration
- Significance: Renal tubular degeneration, kidney disease
Cellular Casts
RBC Casts
- Contain intact red blood cells
- Significance: Glomerulonephritis, renal hemorrhage, infarction
- Highly significant
WBC Casts
- Contain intact white blood cells
- Significance: Pyelonephritis (kidney infection), interstitial nephritis
- Highly significant
Epithelial Casts
- Contain renal epithelial cells
- Significance: Acute tubular necrosis, acute kidney injury
- Highly significant
Waxy Casts
- Smooth, homogeneous, high refractive index
- Represent chronic, advanced degeneration
- Significance: Chronic kidney disease, poor prognosis
Fatty Casts
- Contain fat droplets
- Rare in veterinary patients
- Significance: Nephrotic syndrome, diabetes mellitus, extreme lipiduria
Broad Casts
- 2-3x wider than normal casts
- From dilated, damaged tubules
- Significance: Chronic kidney disease, tubular stasis
Key Concept: Casts indicate RENAL disease. Their presence localizes pathology to the kidneys.
5. CRYSTALS
Clinical Significance: Depends on type, quantity, clinical signs, and urine pH
Common Crystals:
Struvite (Triple Phosphate)
- Appearance: Colorless, “coffin lid” prisms
- pH: Alkaline (>7.0)
- Species: Dogs, cats
- Significance:
- Normal in small numbers
- Large amounts → urolithiasis risk
- Associated with UTI (urease-producing bacteria)
- Dietary management important
Calcium Oxalate
- Appearance: Two forms
- Dihydrate: Colorless “envelope” shape (square with X)
- Monohydrate: Dumbbell or picket-fence shape
- pH: Acidic to neutral
- Species: Dogs, cats (increasing incidence)
- Significance:
- Monohydrate → strongly associated with ethylene glycol (antifreeze) toxicity
- Dietary/genetic predisposition
- Cannot be dissolved medically
Urate (Ammonium Biurate)
- Appearance: Yellow-brown, thorny spheres or “thorn-apple”
- pH: Acidic to neutral
- Species: Dogs (especially Dalmatians, bulldogs), cats
- Significance:
- Portosystemic shunt (liver shunt)
- Severe liver disease
- Dalmatians (genetic)
- High-protein diet
Calcium Phosphate
- Appearance: Amorphous (shapeless) or thin prisms
- pH: Alkaline
- Significance: Usually normal, especially in herbivores
Calcium Carbonate
- Appearance: Small spheres, dumbbell shapes
- Species: Horses, rabbits, guinea pigs
- Significance: NORMAL in herbivores (causes normal cloudiness)
Cystine
- Appearance: Flat, colorless, hexagonal plates
- pH: Acidic
- Species: Dogs (rare genetic disorder)
- Significance:
- Genetic defect in renal tubular reabsorption
- Predisposed breeds: Dachshund, English Bulldog, Newfoundland
- Requires lifelong management
Bilirubin
- Appearance: Yellow-brown needles or granules
- Species: Dogs (small amounts normal), cats (NEVER normal)
- Significance:
- Dogs: Normal in concentrated urine
- Cats: Always pathological (liver disease, hemolysis)
Less Common/Abnormal Crystals:
Sulfonamide Crystals
- From sulfonamide antibiotic administration
- Yellow-brown, sheaves of wheat or rosettes
- Ensure adequate hydration during therapy
Hippuric Acid
- Rare
- Four-sided prisms or needles
Tyrosine
- Fine needles in clusters
- Severe liver disease
Leucine
- Yellow spheres with radial striations
- Severe liver disease
Drug Crystals
- Various antibiotics and medications can crystallize
6. BACTERIA
Normal: None visible in properly collected sample (cystocentesis)
Appearance:
- Cocci (spherical): Chains or clusters
- Rods (bacilli): Short to elongated
Significance:
- Cystocentesis sample: ANY bacteria = UTI (highly significant)
- Catheterized sample: Bacteria may indicate UTI or contamination
- Free-catch sample: Often contamination; interpret with caution
Quantification:
- Few, moderate, or many per HPF
- Heavy bacteriuria often visible even at low power
Clinical Action:
- Pyuria + bacteriuria + clinical signs = perform urine culture and sensitivity
- Do not start antibiotics before culture if possible (affects results)
- Bacteria without WBCs → may be contamination or early infection
Important: Stained sediment (Gram stain, Diff-Quik) improves bacterial visualization
7. FUNGAL ORGANISMS
Candida spp.
- Small budding yeasts with or without pseudohyphae
- Usually contamination or opportunistic infection
- Risk factors: Diabetes, immunosuppression, prolonged antibiotic use
Other Fungi
- Rare in urine
- May indicate systemic fungal infection
8. PARASITES
Capillaria plica (Bladder Worm)
- Appearance: Bi-polar-plugged eggs (lemon-shaped)
- Species: Dogs, cats (rare), foxes
- Significance: Bladder parasitism, hematuria, dysuria
Dioctophyma renale (Giant Kidney Worm)
- Appearance: Large, thick-shelled eggs with rough surface
- Species: Dogs (rare)
- Significance: Kidney destruction
Pearsonema (Capillaria) feliscati
- Species: Cats
- Significance: Bladder parasitism
Microfilaria
- Rare in urine
- Dirofilaria immitis (heartworm) can rarely appear
Stephanurus dentatus
- Kidney worm of pigs
9. MUCUS THREADS
Appearance: Ribbon-like, translucent strands
Significance:
- Normal in small amounts (from urogenital tract)
- Large amounts may indicate inflammation or contamination
- Very common in horses (normal)
10. SPERM
Appearance: Motile or non-motile with characteristic head and tail
Significance:
- Normal in intact males
- Indicates sample from male or contamination in females
- No pathological significance
11. LIPID DROPLETS
Appearance: Highly refractile spheres of various sizes
Significance:
- Small amounts normal, especially in cats
- Large amounts (lipiduria) → nephrotic syndrome, diabetes mellitus, hypothyroidism
- May form fatty casts
12. CONTAMINANTS
Common Contaminants:
- Starch granules: Maltese cross polarization, from glove powder
- Pollen grains
- Fecal material: Free-catch samples
- Hair/fibers
- Air bubbles: Mimic cells; collapsed walls distinguish them
- Calcium oxalate from plants: From herbivore diet.
INTEGRATED INTERPRETATION
Putting It All Together
Complete urinalysis interpretation requires integrating all three components with clinical signs and patient history.
Clinical Scenarios
1. Scenario: Bacterial Cystitis
- Physical: Cloudy, red-tinged urine; USG 1.030
- Chemical: pH 8.5, protein 2+, blood 3+, positive leukocytes
- Microscopic: Many WBCs (50-100/HPF), many RBCs (30-60/HPF), many bacteria, struvite crystals
- Interpretation: Bacterial UTI with struvite crystalluria
- Action: Urine culture, appropriate antibiotics, dietary modification
2. Scenario: Chronic Kidney Disease
- Physical: Pale urine, USG 1.010 (patient is dehydrated)
- Chemical: pH 6.5, protein 2+
- Microscopic: Granular casts (5-10/LPF), few WBCs, few renal epithelial cells
- Interpretation: CKD with isosthenuric urine despite dehydration (critical finding), proteinuria, cylindruria
- Action: Stage kidney disease, check UPC ratio, renal diet, monitor
3. Scenario: Diabetic Ketoacidosis
- Physical: Clear, pale urine; USG 1.025, fruity odor
- Chemical: pH 6.0, glucose 4+, ketones 3+, protein trace
- Microscopic: Rare cells, no significant findings
- Interpretation: DKA – life-threatening emergency
- Action: Immediate hospitalization, IV fluids, insulin, electrolyte monitoring
4. Scenario: Ethylene Glycol Toxicity
- Physical: Clear urine, USG varies (initially high, then drops)
- Chemical: pH acidic, protein variable
- Microscopic: MANY calcium oxalate monohydrate crystals (hippurate, envelope)
- Interpretation: Antifreeze toxicity (emergency)
- Action: Immediate antidote (fomepizole or ethanol), aggressive treatment
5. Scenario: Transitional Cell Carcinoma
- Physical: Red, cloudy urine; USG 1.025
- Chemical: Blood 3+, protein 2+
- Interpretation: Bladder tumor
- Action: Imaging (ultrasound), biopsy, cytology
6. Scenario: Liver Disease (Cat)
- Physical: Dark orange urine, clear; USG 1.045
- Chemical: Bilirubin 3+ (ABNORMAL in cats), pH 6.5
- Microscopic: Bilirubin crystals, no significant cells
- Interpretation: Hepatic or post-hepatic disease
- Action: Liver enzymes, bile acids, imaging, rule out obstruction