What is Rabies?
Rabies is a serious viral infection caused by the RABV virus (Rabies Virus). It’s a deadly disease that affects the nervous system of humans and other warm-blooded animals. While rabies is nearly always fatal once symptoms appear, it is completely preventable with proper treatment after exposure.
Key Facts:
- World Rabies Day is observed annually on September 28th
- About 59,000 people worldwide die from rabies each year
- In the U.S., fewer than 3 people get rabies annually due to effective vaccination programs
- Rabies is found on all continents except Antarctica
Basic Disease Information
| Category | Facts |
|---|---|
| Disease Name | Rabies |
| Causative Agent | Rabies virus (RABV) |
| Virus Family | Rhabdoviridae |
| Virus Type | Single-stranded RNA virus |
| Case Fatality Rate | Nearly 100% once symptoms appear |
| Preventability | 100% preventable with timely post-exposure prophylaxis |
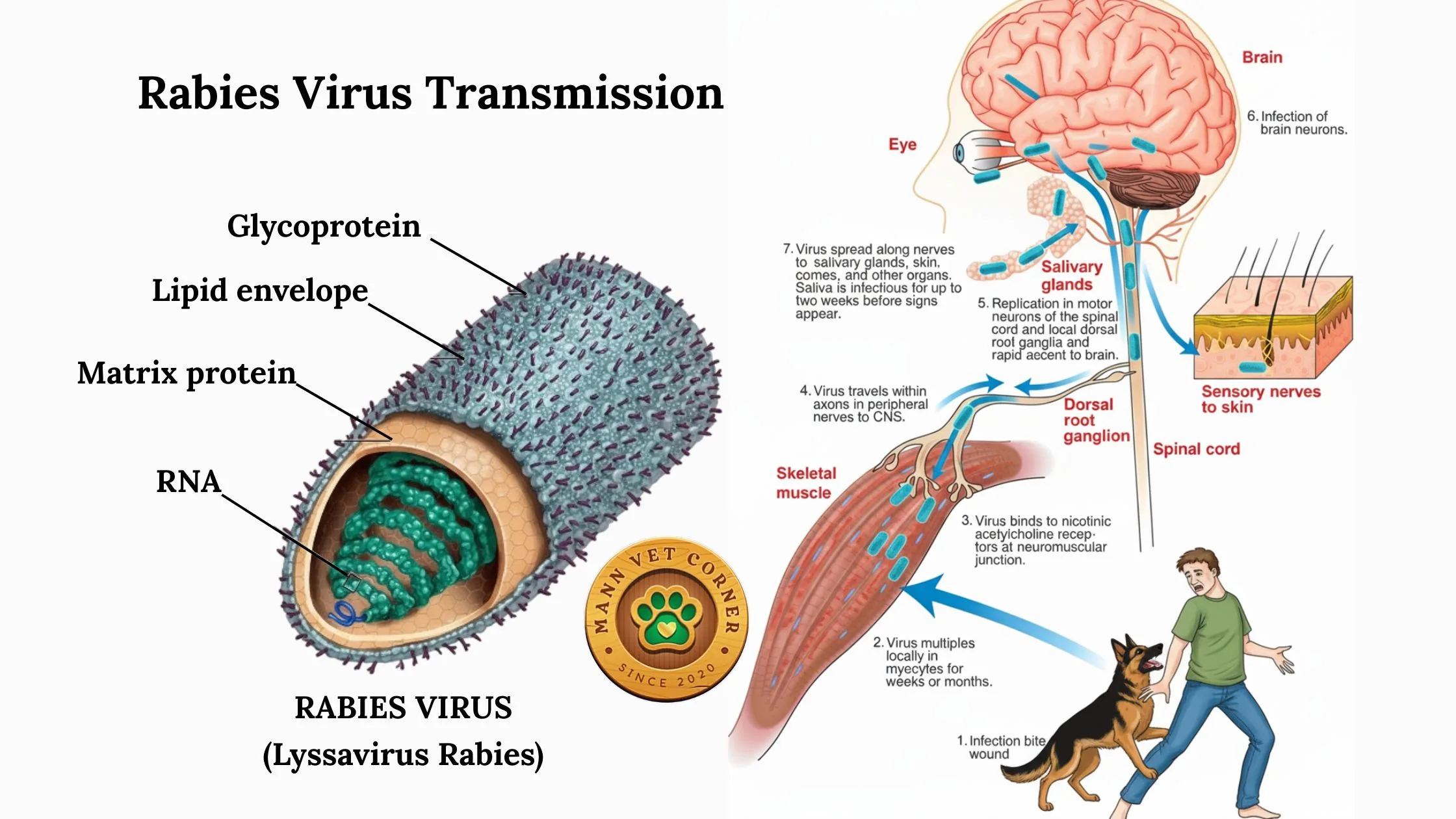
The Rabies Virus (RABV)
The rabies virus belongs to the family Rhabdoviridae. It’s a neurotropic virus, meaning it specifically targets nerve tissue. The virus has a unique ability to hide from the immune system as it travels through the nervous system to reach the brain.
Characteristics:
- Single-stranded RNA virus
- Bullet-shaped appearance under microscopy
- Highly neurotropic (nerve-seeking)
- Present in saliva and nervous system tissue of infected animals
How Rabies Spreads (Transmission)
Rabies transmission occurs through direct contact with infected saliva or nervous system tissue from a rabid animal. The most common ways include:
Primary Routes:
- Animal bites – Most common method (90% of cases)
- Scratches from infected animals
- Contact with mucous membranes (eyes, nose, mouth) through infected saliva
- Open wounds exposed to infected saliva
Transmission Facts
| Transmission Method | Risk Level | Details |
|---|---|---|
| Animal Bite | High | 90% of human cases |
| Scratch from Infected Animal | Moderate | If saliva present |
| Mucous Membrane Contact | Moderate | Eyes, nose, mouth |
| Organ Transplant | Very Rare | Less than 10 documented cases |
| Airborne | Extremely Rare | Only in laboratory/cave settings |
| Person-to-Person | None | Not transmitted between humans |
Rare Routes:
- Organ transplantation from infected donors
- Inhalation of virus particles (extremely rare, in laboratory settings)
Important: Rabies is NOT transmitted through:
- Touching or petting a rabid animal
- Contact with blood, urine, or feces
- Casual contact with infected animals
Animal Hosts
Rabies affects all warm-blooded mammals, but certain animals are more commonly infected:
Animal Hosts by Region
| Location | Primary Hosts | Secondary Hosts |
|---|---|---|
| USA | Bats, raccoons, skunks, foxes | Coyotes, cats, dogs |
| Developing Countries | Domestic dogs | Cats, cattle, monkeys |
| Europe | Bats, foxes | Raccoons (imported) |
| Australia | Bats (lyssavirus) | None (classical rabies-free) |
In the United States:
- Bats (most common source of human rabies)
- Raccoons
- Skunks
- Foxes
- Coyotes
Globally:
- Dogs (responsible for 99% of human rabies deaths worldwide)
- Cats
- Cattle
- Monkeys
Note: In developing countries, particularly in Asia and Africa, domestic dogs are the primary source of human rabies infections.
Global Statistics
| Statistic | Data |
|---|---|
| Annual Global Deaths | Approximately 59,000 people |
| Deaths per Day Worldwide | About 160 people |
| Annual US Cases | Fewer than 3 people |
| Most Affected Regions | Rural Asia and Africa |
| Children at Risk | Higher risk than adults |
| Dog-mediated Deaths | 99% of human rabies deaths globally |
Incubation Period
The incubation period is the time between exposure to the virus and the appearance of symptoms. This varies significantly:
Incubation Period Variables
| Factor | Impact on Incubation | Time Range |
|---|---|---|
| Typical Cases | Standard timeline | 1-3 months |
| Face/Neck Bites | Shorter incubation | 2-8 weeks |
| Hand/Arm Bites | Moderate timeline | 1-3 months |
| Leg Bites | Longer incubation | 3-12 months |
| Severe Bites | Shorter incubation | 2-8 weeks |
| Minor Exposures | Longer incubation | 3 months to 2 years |
Timeline:
- Typical range: 1-3 months
- Possible range: 1 week to several years
- Factors affecting duration:
- Location of bite (closer to brain = shorter incubation)
- Severity of wound
- Amount of virus transmitted
- Individual immune response
Critical Point: During incubation, there are no symptoms, but treatment is still highly effective.

Pathogenesis (How the Disease Develops)
Understanding how rabies progresses in the body helps explain why early treatment is crucial:
1st Stage: Viral Entry and Local Replication
- Virus enters through wound
- Replicates in muscle tissue near bite site
- Can remain localized for days to weeks
2nd Stage: Neural Invasion
- Virus binds to nerve endings
- Travels along peripheral nerves toward spinal cord
- Moves at rate of 12-100mm per day
3rd Stage: Central Nervous System Infection
- Virus reaches spinal cord and brain
- Massive viral replication in brain tissue
- Spreads to salivary glands and other organs
4th Stage: Clinical Disease and Death
- Severe brain dysfunction
- Multiple organ failure
- Death typically within 7-10 days of symptom onset
Signs and Symptoms
Rabies progresses through distinct phases, each with characteristic symptoms:
1. Phase 1: Incubation (No Symptoms)
- Duration: Days to months
- No visible signs of illness
- Virus traveling to brain
2. Phase: Prodromal Phase (Early Symptoms)
- Duration: 2-10 days
- Symptoms:
- Flu-like illness (fever, headache, fatigue)
- Pain, tingling, or numbness at bite site
- Anxiety and agitation
- Difficulty swallowing
3. Phase: Acute Neurologic Phase
This phase has two forms:
Furious Rabies (67% of cases):
- Hyperactivity and agitation
- Hydrophobia (fear of water)
- Aerophobia (fear of air/wind)
- Seizures and hallucinations
- Aggressive behavior
- Duration: 2-7 days
Paralytic Rabies (33% of cases):
- Progressive paralysis starting from bite site
- Muscle weakness
- Loss of coordination
- Duration: Up to 30 days
Phase 4: Coma and Death
- Deep coma
- Respiratory failure
- Cardiac arrest
- Death within days
Clinical Phases
| Phase | Duration | Key Symptoms | Outcome |
|---|---|---|---|
| Incubation | Days to months | None | Treatable |
| Prodromal | 2-10 days | Flu-like, bite site pain | Too late for treatment |
| Acute Neurologic | 2-30 days | Furious or paralytic rabies | Fatal |
| Coma | 1-7 days | Unconsciousness | Death |
Prevention
Prevention is the key to avoiding rabies, as there’s no cure once symptoms appear.
Pre-Exposure Prevention
For High-Risk Individuals:
- Veterinarians
- Animal control officers
- Laboratory workers
- Travelers to high-risk areas
- Vaccination: 2-dose series with boosters as needed
Vaccination Schedule
| Type | Timeline | Doses | Effectiveness |
|---|---|---|---|
| Pre-Exposure | Day 0, Day 7 | 2 doses | 99%+ |
| Post-Exposure (Previously Vaccinated) | Day 0, Day 3 | 2 doses | Nearly 100% |
| Post-Exposure (Unvaccinated) | Days 0, 3, 7, 14 | 4 doses + RIG | Nearly 100% |
| Booster (High Risk) | Every 2-5 years | 1 dose | Maintains immunity |
Post-Exposure Prevention
Immediate Actions:
- Wound care: Clean thoroughly with soap and water for 15 minutes
- Medical attention: Seek immediate healthcare
- Report incident: Contact local health authorities
Medical Treatment:
- Post-Exposure Prophylaxis (PEP): Series of rabies vaccinations
- Rabies Immune Globulin (RIG): Antibodies injected around wound
- Timeline: Must begin as soon as possible after exposure
General Prevention Measures
- Vaccinate pets and livestock
- Avoid contact with wild animals
- Never approach or feed wild animals
- Secure garbage and pet food
- Install bat-proofing in buildings
- Report strange animal behavior to authorities
Treatment
Before Symptoms Appear
Post-Exposure Prophylaxis (PEP) is nearly 100% effective when given promptly:
Standard Protocol:
- Day 0: Rabies vaccine dose 1 + Rabies Immune Globulin (if not previously vaccinated)
- Day 3: Rabies vaccine dose 2
- Day 7: Rabies vaccine dose 3
- Day 14: Rabies vaccine dose 4
Side Effects (usually mild):
- Pain at injection site
- Low-grade fever
- Muscle aches
- Nausea
After Symptoms Appear
Unfortunately, there is no effective treatment once rabies symptoms develop. The disease is nearly always fatal at this stage. This is why prevention and immediate post-exposure treatment are so critical.
Supportive Care:
- Intensive care management
- Pain control
- Sedation for agitation
- Respiratory support

World Rabies Day 2025
World Rabies Day, observed on September 28th, aims to raise awareness about rabies prevention and elimination. The 2025 theme focuses on achieving the global goal of eliminating dog-mediated human rabies deaths by 2030.
Key Messages for 2025:
- Rabies is 100% preventable but nearly 100% fatal
- Dog vaccination is the most cost-effective prevention strategy
- Immediate medical attention after animal bites saves lives
- Global collaboration is essential for rabies elimination
World Rabies Day Facts
| Aspect | Information |
|---|---|
| Date | September 28 annually |
| Established | 2007 |
| Purpose | Raise awareness and promote prevention |
| 2025 Theme | Eliminating dog-mediated human rabies |
| Target Goal | Zero human rabies deaths by 2030 |
| Organizations | WHO, OIE, FAO, GARC |
Important Reminders
Seek Medical Attention Immediately If:
- You’re bitten or scratched by any wild animal
- You’re bitten by an unknown domestic animal
- You have contact with bats (even without obvious bite)
- An animal bite breaks the skin
- You’re traveling to high-risk areas
Remember:
- Rabies is preventable with proper treatment
- Time is critical – don’t wait for symptoms
- When in doubt, seek medical advice
- Prevention is always better than treatment
Emergency Contact: If exposed to potentially rabid animals, contact your healthcare provider or local emergency department immediately. Rabies exposure is considered a medical emergency.