Insight into Life Cycle, Clinical Signs, Prevention, Treatment in Humans and Animals
Botflies represent one of nature’s most unsettling parasites. These insects affect both humans and animals worldwide, causing significant discomfort and health concerns. Botflies can endanger animals and humans, primarily through their parasitic larval stage, which causes a condition called myiasis. While many infestations are treatable, severe complications can occur, leading to pain, secondary infections, and in rare cases, life-threatening conditions or even death. This comprehensive guide explores botfly infestations, their life cycle, clinical signs, and effective treatment strategies.
What Are Botflies? Understanding These Parasitic Insects
Botflies belong to the Oestridae family, comprising over 150 species of parasitic flies. These insects complete their larval development inside living mammals, including humans, dogs, cats, horses, cattle, and wildlife. Unlike mosquitoes that simply bite and leave, botflies deposit their larvae beneath the skin, where they develop over several weeks.
The most common species affecting humans is Dermatobia hominis, known as the human botfly. This species primarily inhabits Central and South America, though travelers can bring infestations back to other regions.
Why Botflies Matter to Pet Owners and Travelers
Veterinarians report thousands of botfly cases annually in domestic animals. Pet owners living in or traveling to endemic areas face real risks. Understanding botfly behavior helps you protect your family and pets from these parasites.
Botflies in Humans: How Human Botfly Infestations Occur
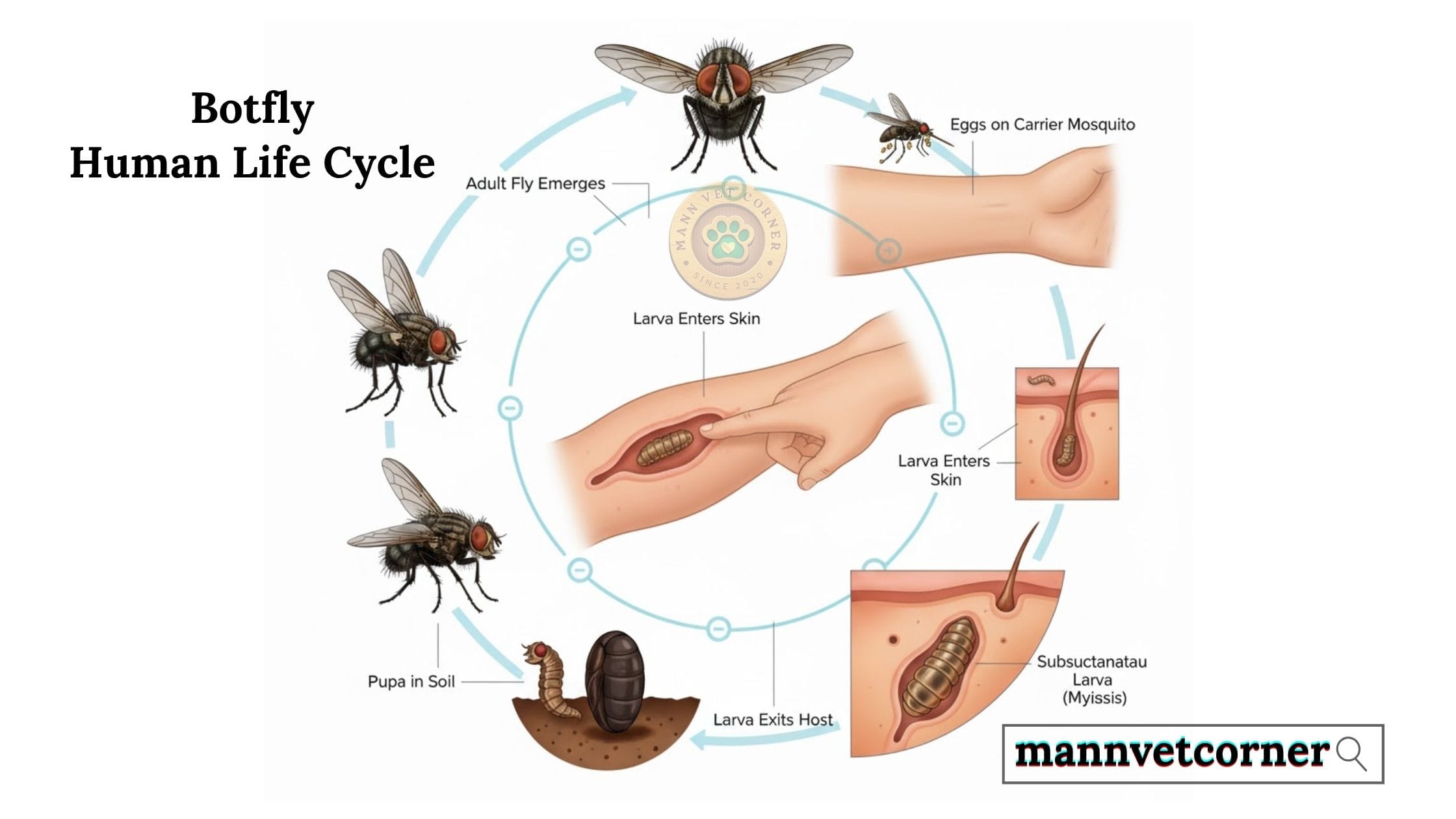
Botflies, particularly the human botfly (Dermatobia hominis), are parasitic insects that can infest humans, leading to painful lesions and requiring medical intervention for removal. Human botfly infestations, medically termed myiasis, occur when larvae penetrate skin and develop subcutaneously. The human botfly employs a unique transmission method that makes prevention challenging.
Transmission Methods in Human Hosts
The female botfly captures mosquitoes or other blood-feeding insects mid-flight and attaches her eggs to their bodies. When these carrier insects land on human skin to feed, body heat triggers the botfly eggs to hatch. The larvae then drop onto the skin and burrow into hair follicles or small wounds within minutes.
This clever strategy allows botflies to infect hosts without direct contact. Many people never realize they’ve been exposed until symptoms develop days later.
Common Geographic Risk Areas for Human Botfly Exposure
Human botfly infestations occur most frequently in:
- Central American countries including Costa Rica, Panama, and Belize
- South American nations such as Brazil, Colombia, and Argentina
- Parts of Mexico, particularly rural and forested regions
- Caribbean islands with tropical climates
Travelers to these regions should take preventive measures seriously, especially when engaging in outdoor activities like hiking, camping, or wildlife observation.
Botflies in Animals: Domestic and Wild Host Species
They are parasitic insects that lay their larvae in or on mammals, causing various health issues, particularly in small animals like dogs and rodents. Botflies infest numerous animal species, with different botfly varieties specializing in particular hosts. Understanding which animals face the greatest risk helps owners implement targeted prevention strategies.
Botflies in Dogs: Canine Cuterebra Infestations
Dogs encounter botflies primarily through outdoor exploration. The North American species Cuterebra commonly affects canines, particularly hunting dogs and those frequenting wooded areas.
Dogs typically pick up botfly larvae when investigating rabbit or rodent burrows. The larvae quickly penetrate the dog’s skin, often around the head, neck, or trunk. Once established, the larva creates a breathing hole (warble) visible as a small opening in the skin.
High-Risk Dog Activities:
- Exploring rabbit warrens or rodent holes
- Running through tall grass or brush
- Hunting in forested environments
- Playing near wildlife habitats during summer months
Botflies in Cats: Feline Cuterebra Cases
Cats face similar botfly risks as dogs, though feline cases often present more dramatically. Outdoor cats hunting small prey frequently encounter Cuterebra larvae in their natural habitat.
Curious cats investigating burrows may inadvertently contact larvae. The parasites typically lodge in the cat’s neck, head, or thorax regions. Some cats develop neurological complications if larvae migrate aberrantly into body cavities or the nervous system.
Warning Signs in Cats:
- Sudden lethargy or behavioral changes
- Visible lumps with central breathing holes
- Excessive grooming of specific areas
- Unexplained swelling or abscess-like formations
Other Susceptible Hosts: Livestock and Wildlife
Beyond companion animals, botflies affect:
Livestock Species:
- Cattle suffer from heel flies (Hypoderma species) that damage hides and reduce productivity
- Horses host nasal botflies that deposit larvae in the mouth and migrate to the stomach
- Sheep and goats experience similar infestations causing economic losses
Wildlife Populations:
- Rabbits and rodents serve as primary hosts for Cuterebra species
- Deer host several botfly varieties
- Squirrels frequently carry botfly larvae during warmer months
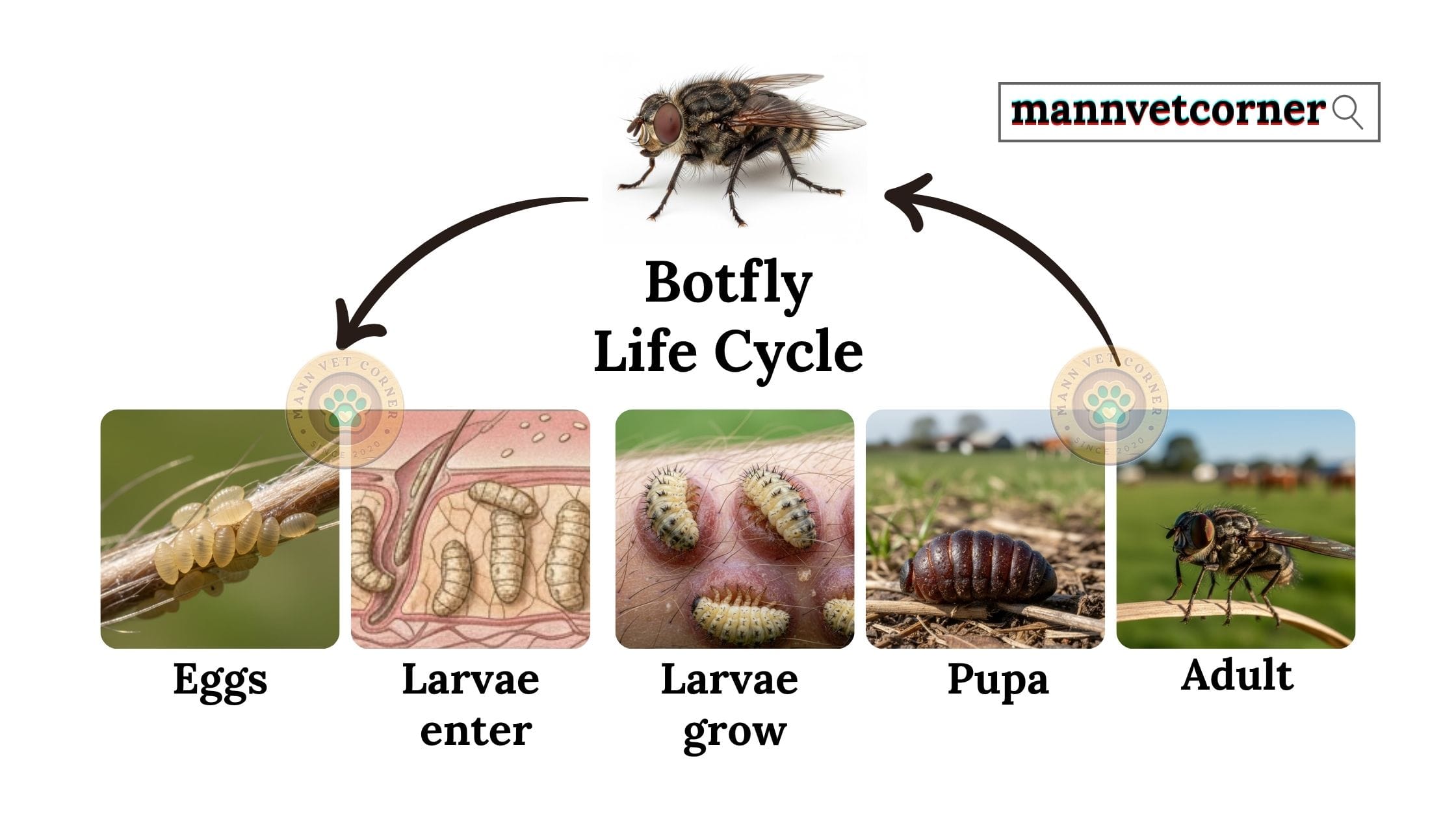
The Botfly Life Cycle: From Egg to Adult Emergence
The lifecycle of a botfly involves several distinct stages: egg, larva, pupa, and adult, with a parasitic relationship with warm-blooded hosts. Understanding the botfly life cycle reveals critical intervention points for prevention and treatment. The complete cycle spans several weeks to months, depending on species and environmental conditions.
Stage One: Egg Deposition and Hatching
Adult female botflies employ various reproductive strategies. Some species attach eggs directly to host hair. Others, like the human botfly, use intermediate carriers such as mosquitoes. The female captures these insects and glues her eggs to their abdomens.
Eggs remain dormant until environmental triggers activate them. For species using carriers, body heat from the next blood meal stimulates hatching. Direct-laying species respond to host proximity or physical contact.
Stage Two: Larval Penetration and Development
Newly hatched first-instar larvae measure less than 1 millimeter. They actively seek entry points through:
- Hair follicles providing natural passages
- Minor skin abrasions or cuts
- Mucous membranes in nasal or oral passages
Once beneath the skin, larvae excavate pockets called warbles. They molt through three distinct developmental stages (instars), growing substantially with each transformation. The developing larva maintains a breathing hole at the skin surface, often visible as a small puncture with seepage.
Timeline of Larval Development:
- Week 1-2: First instar establishment and initial growth
- Week 3-4: Second instar development and warble expansion
- Week 5-8: Third instar maturation and preparation for emergence
- Week 8-10: Exit from host and pupation in soil
Stage Three: Emergence and Pupation
Mature third-instar larvae exit through their breathing holes, dropping to the ground. This emergence often occurs at night when the host rests. The larvae burrow into soil or leaf litter, forming protective pupae.
Pupation duration varies by species and temperature, typically lasting 3-12 weeks. Adult flies emerge, mate, and restart the cycle. Adults live only days to weeks, focusing entirely on reproduction.
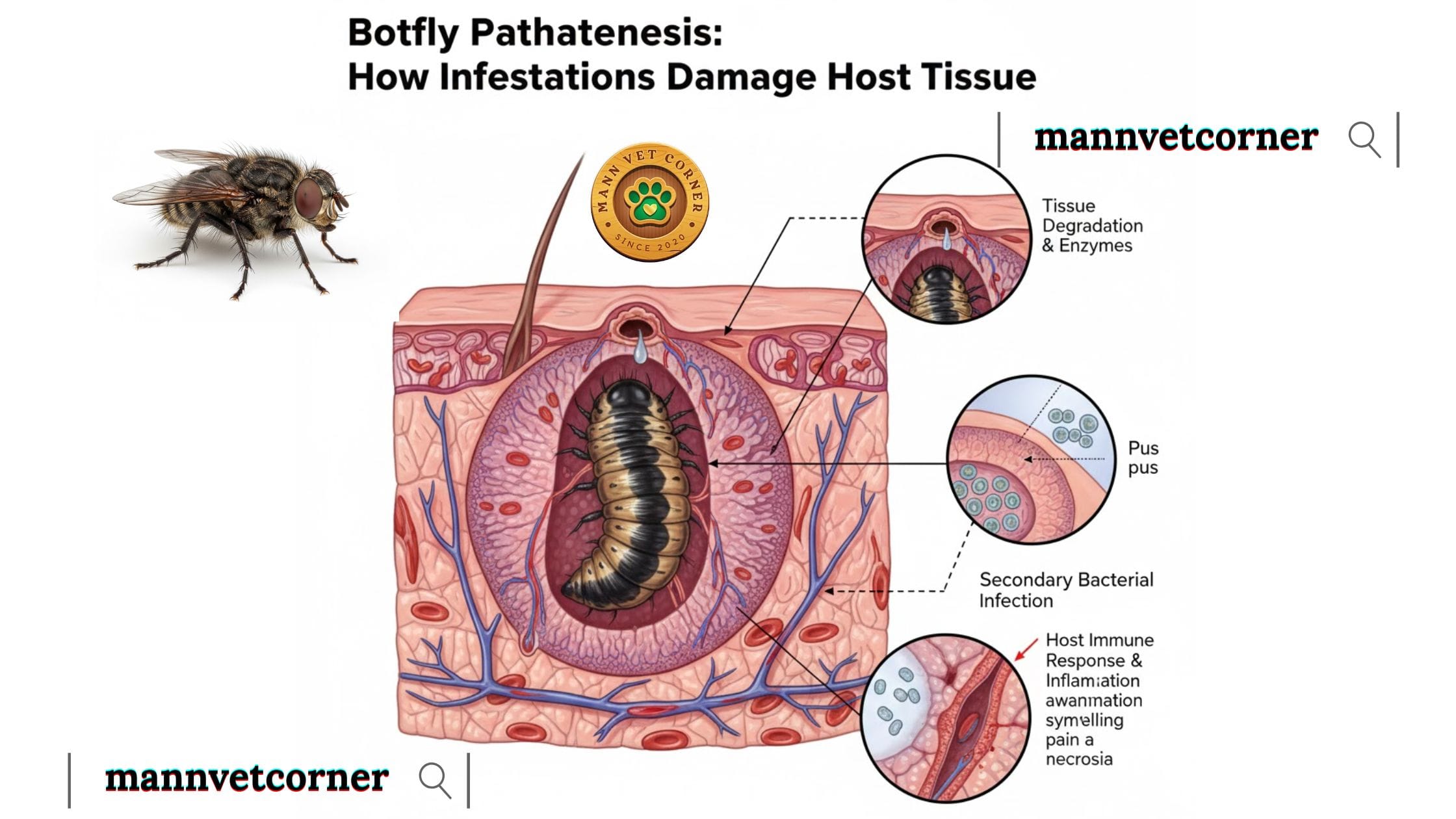
Botfly Pathogenesis: How Infestations Damage Host Tissue
To reproduce, these flies depend on a process known as myiasis, which involves infesting a host’s skin to feed their larvae. If you’re infested by a bot fly, the issue usually resolves on its own within six weeks. During this time, the bot fly matures and leaves the host’s body on its own. Botfly larvae cause tissue damage through multiple mechanisms. Understanding the pathogenesis helps predict complications and guide treatment approaches.
Mechanical Tissue Destruction
Growing larvae physically displace tissue, creating cavities up to 2 centimeters in diameter. This mechanical pressure destroys surrounding cells and disrupts normal tissue architecture. The breathing hole provides a portal for secondary bacterial infections, which significantly complicate healing.
Inflammatory Response and Immune Reactions
The host immune system recognizes botfly larvae as foreign invaders, triggering intense inflammatory responses. White blood cells accumulate around the warble, producing pus and causing swelling. This inflammation serves protective purposes but also contributes to discomfort and tissue damage.
Some hosts develop hypersensitivity reactions to larval secretions, causing exaggerated immune responses. These allergic reactions manifest as extensive swelling, pain, and systemic symptoms.
Secondary Complications and Infections
Bacterial contamination through the breathing hole creates abscess-like conditions. Common bacterial invaders include Staphylococcus and Streptococcus species. These infections extend tissue damage beyond the immediate warble area.
Rare but serious complications occur when larvae migrate aberrantly:
- Neurological damage from brain or spinal cord invasion
- Respiratory compromise from tracheal involvement
- Ocular damage affecting vision
- Visceral migration causing organ dysfunction
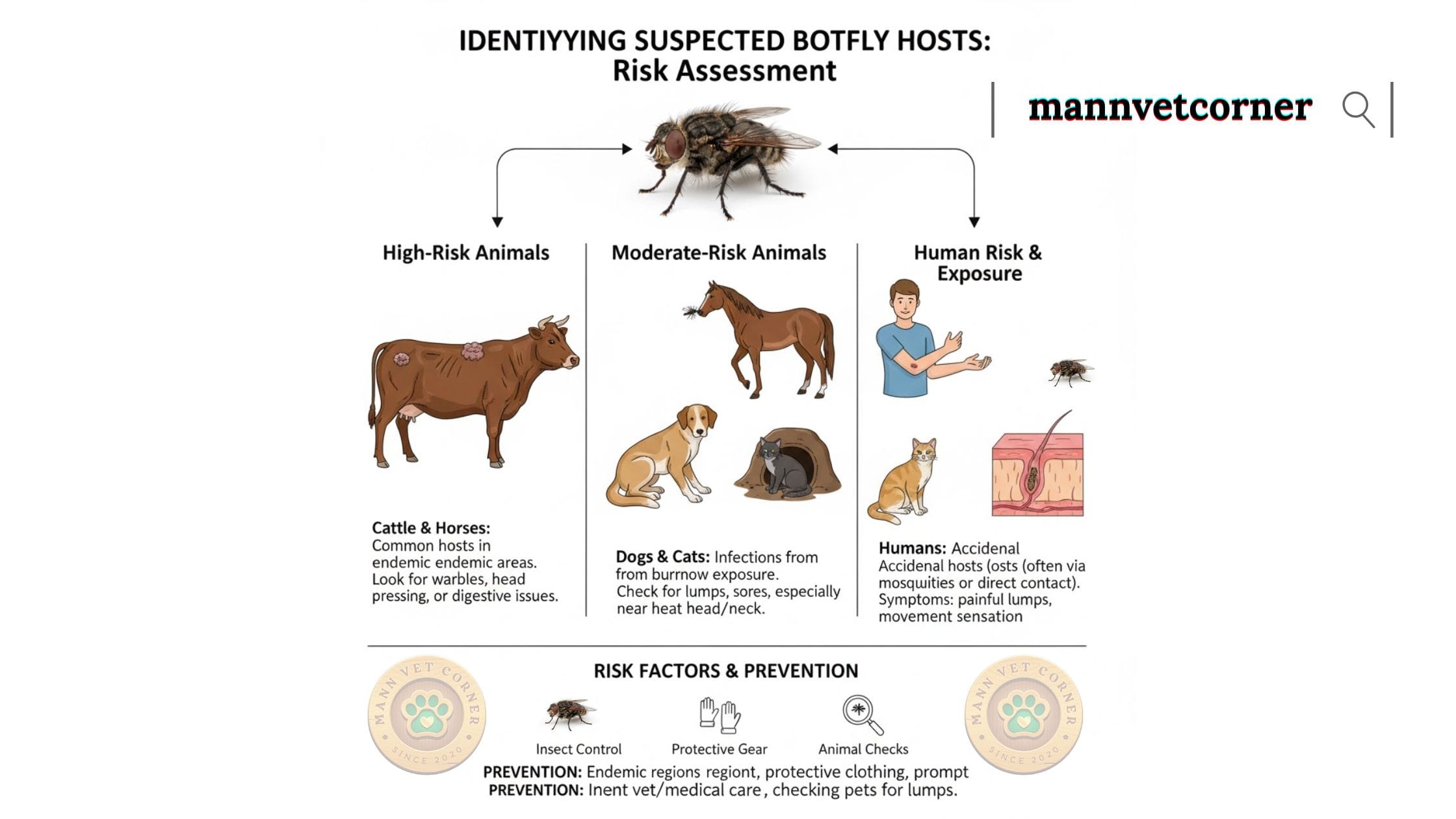
Identifying Suspected Botfly Hosts: Risk Assessment
Timely laboratory data is essential for accurate risk assessment. Meteorological and environmental monitoring services supply weather data and climate indicators that influence bot fly life cycles. Determining which individuals or animals face botfly exposure risks helps prioritize preventive measures and early detection efforts.
Geographic and Seasonal Risk Factors
Endemic Regions:
- Tropical and subtropical zones year-round
- Temperate regions during warmer months (late spring through early fall)
- Areas with abundant wildlife populations serving as reservoir hosts
Seasonal Patterns: Botfly activity peaks when temperatures consistently exceed 15°C (59°F). In temperate climates, infestations concentrate between May and September. Tropical regions experience activity throughout the year, with slight increases during rainy seasons when mosquito populations surge.
Behavioral and Environmental Exposures
High-Risk Human Behaviors:
- Outdoor recreation in endemic areas
- Agricultural work in affected regions
- Wildlife research or observation
- Travel to rural tropical destinations
- Camping without adequate protective measures
High-Risk Animal Activities:
- Free-roaming outdoor access for pets
- Hunting or working dogs in wildlife areas
- Livestock grazing in botfly-endemic pastures
- Wildlife rehabilitation work
Pre-Existing Health Conditions
Immunocompromised individuals face greater complication risks from botfly infestations. Conditions affecting immune function include:
- HIV/AIDS
- Diabetes mellitus
- Cancer undergoing chemotherapy
- Chronic corticosteroid use
- Organ transplant recipients on immunosuppressants
Similarly, animals with weakened immune systems experience more severe infestations and complications.
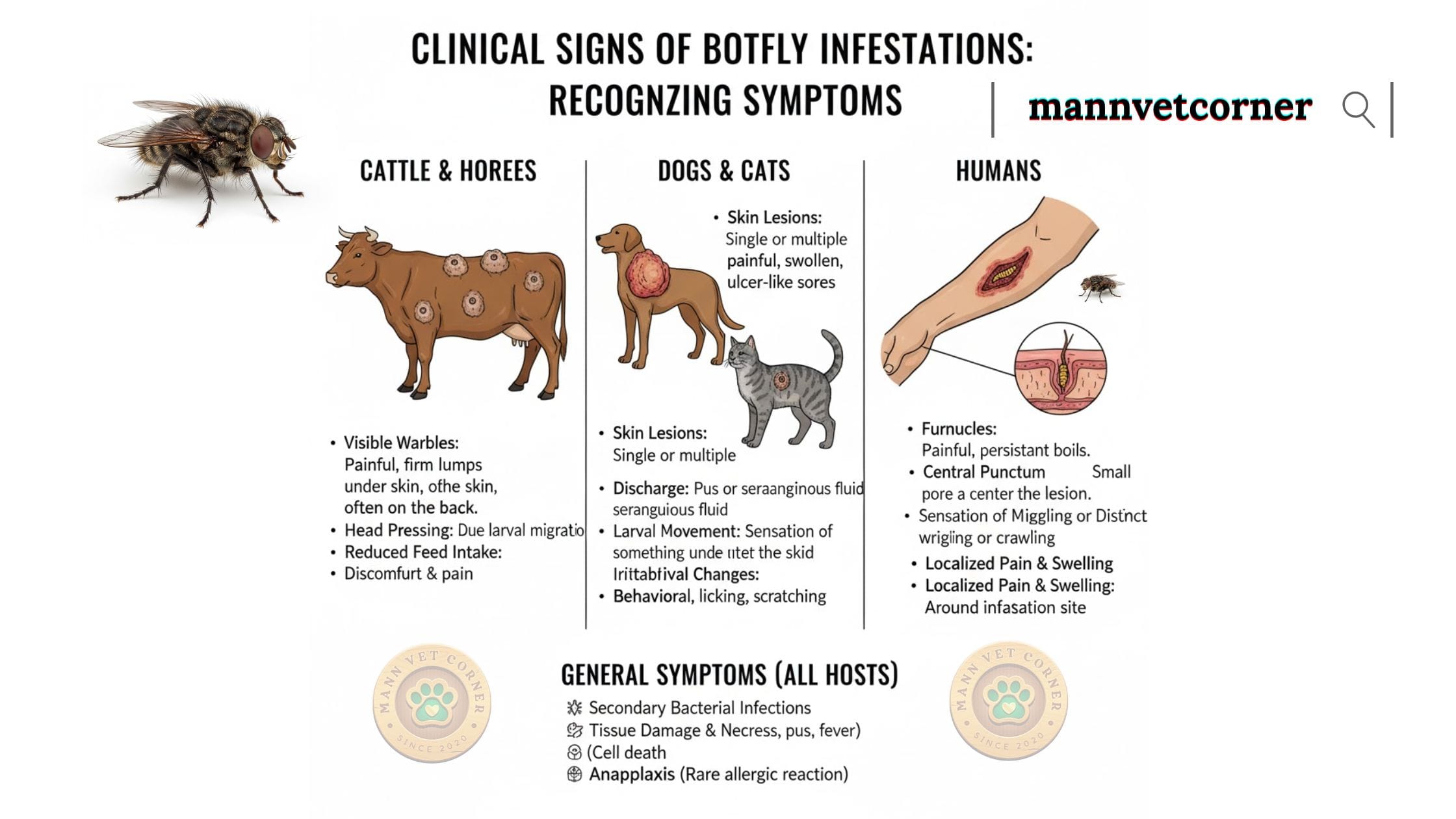
Clinical Signs of Botfly Infestations: Recognizing Symptoms
The main symptoms of a botfly infestation include itching, swelling, a foul odor, and even a sensation of movement under the skin. In some cases, bleeding and loss of appetite may also occur as the larvae grow. Early recognition significantly improves treatment outcomes. Clinical signs vary by host species, infestation location, and individual immune responses.
Signs in Humans
Early Stage Symptoms (Days 1-7):
- Mild itching at penetration site
- Small red bump resembling an insect bite
- Occasional stinging or crawling sensations
- Minor localized swelling
Middle Stage Symptoms (Weeks 2-5):
- Visible breathing hole appearing as a dark central punctum
- Intermittent sharp pains when larva moves
- Increasing swelling and redness around warble
- Serous or serosanguineous discharge from opening
- Firm nodule palpable beneath skin
- Disturbing sensations of movement under skin
Late Stage Symptoms (Weeks 6-10):
- Large raised lesion up to 2-3 centimeters
- Visible larval movement at breathing hole
- Secondary bacterial infection signs (increased pain, purulent discharge, fever)
- Lymph node swelling in regional drainage areas
Signs in Dogs
Observable Canine Indicators:
- Visible lump with central hole, often on head, neck, or flanks
- Excessive licking or scratching at affected area
- Behavioral changes indicating discomfort
- Matted fur around warble from discharge
- Fever in cases with secondary infection
- Lethargy or appetite loss with systemic involvement
Critical Warning Signs:
- Respiratory distress if larvae affect nasal passages
- Neurological symptoms (seizures, weakness, incoordination) indicating aberrant migration
- Sudden collapse or severe pain
Signs in Cats
Feline-Specific Presentations:
- Similar warble formations as dogs but often on head or neck
- Pronounced behavioral changes (hiding, aggression from pain)
- Vocalization when touching affected area
- Neurological symptoms more common than in dogs due to smaller body size
Emergency Feline Symptoms:
- Seizures or altered consciousness
- Sudden blindness
- Paralysis or severe weakness
- Difficulty breathing
Signs in Livestock
Cattle Warbles:
- Multiple lumps along back (hence “heel flies”)
- Hide damage reducing leather quality
- Decreased milk production in dairy cattle
- Weight loss and reduced growth rates
- Behavioral changes during fly season
Horse Botfly Signs:
- Eggs visible attached to leg hairs
- Oral discomfort or irritation
- Gastric symptoms after larvae reach stomach
- Weight loss with heavy infestations
- Colic episodes in severe cases
Clinical Diagnosis of Botfly Infestations: Medical Assessment
Accurate diagnosis combines clinical examination, patient history, and sometimes additional diagnostic procedures. Most cases receive diagnoses through characteristic clinical presentations. Diagnosing bot fly myiasis, an infection caused by a type of fly larva, often involves using ultrasound. This imaging tool can help the doctor identify a brighter, or ‘hyperechoic’, mass just beneath the surface of the skin that blocks, or ‘casts a shadow’ on, the deeper structures underneath it.
Physical Examination Findings
Veterinarians and physicians diagnose botfly myiasis by identifying pathognomonic features:
Definitive Diagnostic Signs:
- Furuncular lesion with central breathing pore
- Movement observed at the opening
- Sensation of larval motion on palpation
- Serosanguineous discharge from punctum
- Firm subcutaneous nodule
Gentle pressure around the warble may reveal the larva at the opening. Healthcare providers avoid excessive manipulation that might rupture the larva, as this releases antigens triggering anaphylactic reactions.
Patient History Assessment
Comprehensive history-taking establishes exposure risk:
Essential Historical Information:
- Recent travel to endemic regions
- Outdoor activity patterns
- Timeline of lesion development
- Associated symptoms (pain, fever, discharge)
- Previous similar episodes
- Immunization status and underlying health conditions
For animals, owners provide information about:
- Outdoor access and typical environments
- Recent behavioral changes
- Travel history or new geographic exposures
- Previous parasite prevention measures
Differential Diagnosis Considerations
Healthcare providers distinguish botfly myiasis from conditions presenting similarly:
Conditions Mimicking Botfly Infestations:
- Bacterial abscesses or furuncles
- Foreign body reactions
- Sebaceous cysts becoming infected
- Other parasitic infections (tungiasis, leishmaniasis)
- Neoplastic lesions
- Actinomycosis or other deep fungal infections
Definitive diagnosis occurs when providers extract and identify the larva. Microscopic examination confirms species identification through characteristic morphological features.
Advanced Diagnostic Methods
Complex or atypical cases may require additional diagnostic tools:
Imaging Studies:
- Ultrasound visualizes larvae within warbles, useful when breathing holes are not apparent
- CT or MRI scans locate aberrantly migrating larvae causing neurological symptoms
- Radiographs occasionally identify larvae in nasal passages or sinuses
Laboratory Testing:
- Complete blood count may show eosinophilia (elevated eosinophils) suggesting parasitic infection
- Culture of discharge identifies secondary bacterial infections
- Histopathological examination of excised tissue confirms diagnosis in unclear cases
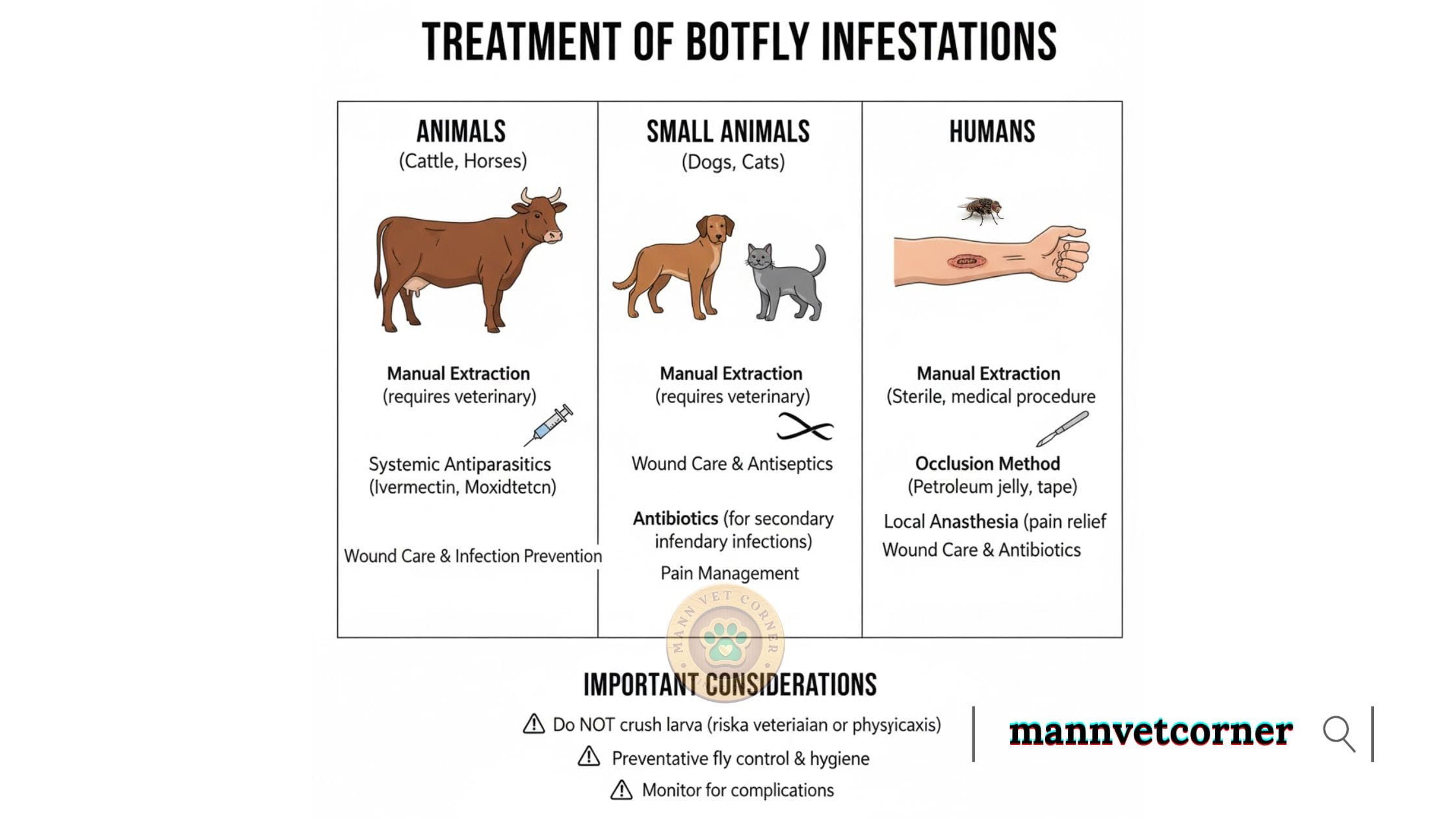
Treatment of Botfly Infestations: Medical and Surgical Approaches
Effective treatment removes larvae completely while minimizing tissue damage and preventing complications. To treat a botfly infestation, the primary method is to remove the botfly larva. This is the only effective treatment, as antibiotics and other medications are ineffective. After removal, it is important to treat the area with an antibiotic ointment to prevent bacterial infection. In some cases, corticosteroids may be prescribed to manage itching. Treatment approaches depend on infestation location, host health status, and available resources.
Manual Extraction: The Primary Treatment Method
Complete larval removal represents the definitive cure for botfly myiasis. Healthcare providers and veterinarians employ careful techniques to extract larvae intact.
Extraction Procedure Steps:
- Preparation Phase:
- Clean the affected area with antiseptic solution
- Inject local anesthetic around the warble for pain control
- Prepare sterile forceps and other extraction instruments
- Occlusion Technique:
- Cover the breathing hole with petroleum jelly, bacon strips, or adhesive tape
- This suffocates the larva, forcing it to emerge for air over 30-60 minutes
- Works best for superficial, easily accessible lesions
- Surgical Extraction:
- Enlarge the breathing hole with a small incision if needed
- Use fine forceps to grasp the larva’s posterior end when visible
- Apply steady, gentle traction to remove the larva intact
- Avoid crushing the larva, which releases allergenic proteins
- Post-Extraction Care:
- Irrigate the cavity thoroughly with saline solution
- Apply topical antibiotics to prevent secondary infection
- Leave wound open for drainage rather than closing primarily
- Prescribe oral antibiotics if bacterial infection is present
Critical Extraction Principles:
- Extract larvae completely; retained fragments cause granulomatous reactions
- Avoid excessive force that ruptures the larva
- Ensure all spines and hooks are removed from tissue
- Confirm no additional larvae in multi-parasite infestations
Pharmacological Treatment Options
Medications serve adjunctive roles in botfly management, though mechanical removal remains essential.
Ivermectin Therapy:
- Systemic ivermectin kills botfly larvae
- Dosing: 200 mcg/kg orally as single dose for humans
- Veterinary dosing varies by species and product
- Useful when extraction proves impossible or larvae are inaccessible
- Dead larvae still require removal to prevent abscess formation
Antibiotic Coverage:
- Broad-spectrum antibiotics treat secondary bacterial infections
- First-generation cephalosporins or amoxicillin-clavulanate commonly prescribed
- Duration: 7-10 days for complicated cases
- Topical antibiotics applied to extraction sites
Analgesics and Anti-inflammatories:
- NSAIDs reduce pain and swelling during and after treatment
- Stronger analgesics may be needed for extensive infestations
- Corticosteroids occasionally used for severe inflammatory reactions
Treatment of Complications
Complicated cases require specialized interventions:
Neurological Involvement:
- Corticosteroids reduce brain or spinal cord inflammation
- Surgical neurosurgical removal if larvae are accessible
- Anticonvulsants for seizure control
- Supportive care and monitoring in hospital settings
Ocular Botfly Myiasis:
- Ophthalmological consultation essential
- Surgical removal under microscopic visualization
- Topical and systemic steroids prevent vision-threatening inflammation
- Antibiotic prophylaxis
Secondary Infections:
- Culture-guided antibiotic therapy
- Abscess drainage if needed
- Wound care management
- Tetanus prophylaxis in unvaccinated individuals
Veterinary Treatment Considerations
Animal treatment follows similar principles with species-specific modifications:
Anesthesia Requirements:
- Cats and dogs often require sedation or general anesthesia for extraction
- Restraint must prevent patient movement during delicate procedures
- Monitoring throughout recovery period
Post-Treatment Care:
- Elizabethan collars prevent licking of wounds
- Follow-up examinations ensure complete healing
- Watch for signs of recurrence or additional larvae
- Pain management appropriate to species
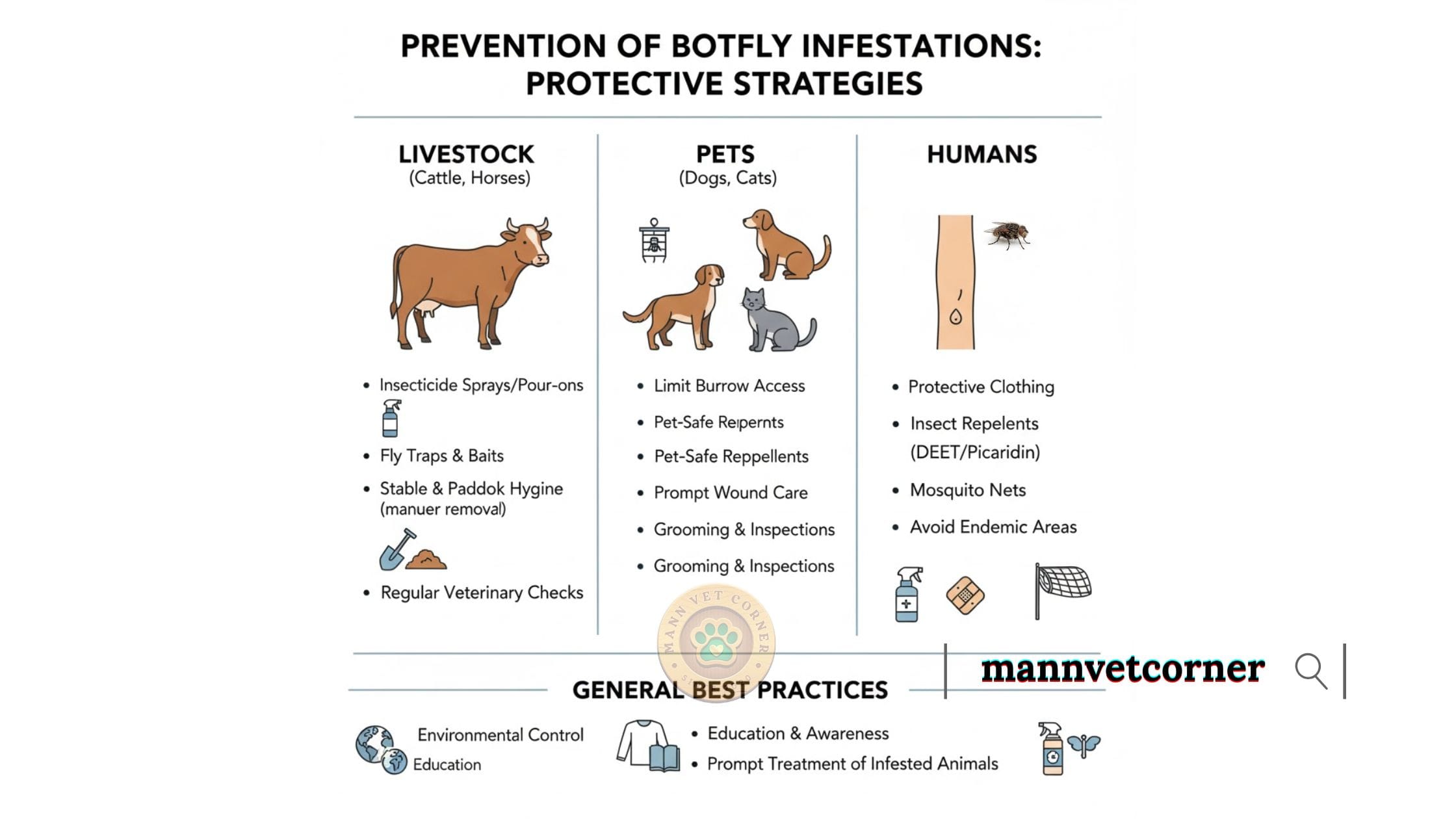
Prevention of Botfly Infestations: Protective Strategies
Prevention provides the most effective approach to avoiding botfly-related health problems. To prevent botfly infestations, use insect repellents, maintain cleanliness, and wear protective clothing when in areas where botflies are prevalent.
Comprehensive strategies address environmental, behavioral, and chemical protection methods.
Personal Protection for Humans
Travelers to endemic regions should implement multiple preventive layers:
Clothing-Based Protection:
- Wear long-sleeved shirts and long pants in outdoor environments
- Choose light-colored clothing making mosquitoes and flies more visible
- Tuck pants into boots or socks to prevent access to skin
- Consider permethrin-treated clothing for enhanced protection
Insect Repellent Use:
- Apply DEET-based repellents (20-30% concentration) to exposed skin
- Reapply every 4-6 hours or per product instructions
- Use picaridin or IR3535 as DEET alternatives
- Apply repellents to clothing as well as skin
- Ensure complete coverage, especially on neck and extremities
Environmental Awareness:
- Avoid known botfly habitat during peak activity periods
- Inspect body for unusual bites or bumps after outdoor activities
- Sleep under mosquito nets in endemic areas
- Use screened lodging when available
Protecting Dogs from Botfly Infestations
Dog owners in affected regions must balance outdoor enrichment with parasite prevention:
Behavioral Modifications:
- Supervise outdoor activities during botfly season
- Discourage investigation of rabbit burrows and rodent holes
- Keep dogs away from known wildlife concentration areas
- Limit exposure during peak activity times (warm afternoons)
Preventive Products:
- Monthly topical or oral parasiticides with insecticidal properties
- Products containing fipronil, selamectin, or moxidectin provide some protection
- Consult veterinarians about product selection for specific regions
- Maintain consistent year-round prevention in endemic areas
Regular Inspection:
- Check dogs thoroughly after outdoor activities
- Pay special attention to head, neck, and trunk areas
- Look for small breathing holes or developing lumps
- Early detection allows simpler treatment
Protecting Cats from Botfly Exposure
Feline prevention focuses on reducing outdoor access during high-risk periods:
Indoor/Outdoor Management:
- Keep cats indoors during botfly season if possible
- Supervise outdoor time in enclosed areas
- Prevent hunting behaviors that lead to burrow exploration
- Provide enrichment to satisfy predatory instincts indoors
Preventive Medications:
- Selamectin (Revolution) provides broad-spectrum parasite control including some fly protection
- Monthly application during warm months
- Year-round prevention in tropical climates
Monitoring and Inspection:
- Weekly full-body checks for outdoor cats
- Immediate veterinary attention for suspicious lumps
- Watch for behavioral changes suggesting discomfort
Livestock Protection Strategies
Agricultural producers implement integrated pest management approaches:
Environmental Management:
- Pasture rotation reduces parasite exposure
- Remove standing water breeding mosquitoes and other carriers
- Maintain fence lines and eliminate tall grass near barns
- Time grazing to avoid peak fly activity periods
Chemical Control:
- Pour-on insecticides for cattle (permethrin, cypermethrin products)
- Oral ivermectin or eprinomectin for systemic protection
- Insecticide ear tags during fly season
- Strategic treatment timing based on regional botfly lifecycle
Monitoring Programs:
- Regular herd checks for warbles
- Systematic treatment of affected animals
- Record-keeping to identify high-risk pastures or time periods
- Veterinary consultation for persistent problems
Community and Environmental Approaches
Broader prevention strategies reduce regional botfly populations:
Public Health Measures:
- Education programs about botfly risks and prevention
- Traveler advisories for endemic destinations
- Healthcare provider training for recognition and treatment
- Surveillance systems tracking infestation patterns
Vector Control:
- Mosquito population management reduces human botfly transmission
- Area-wide insecticide applications in severe outbreak situations
- Wildlife management where appropriate
- Research into botfly-specific control methods
Understanding Geographic Distribution and Epidemiology
Botfly distribution follows specific geographic and ecological patterns. Understanding these helps predict risk and target prevention efforts.
Global Distribution Patterns
Americas:
- Human botfly (Dermatobia hominis): Mexico through Argentina
- Cuterebra species: Throughout North America
- Highest prevalence in Central and South America
- Seasonal occurrence in temperate North America
Other Regions:
- Africa: Several species affecting humans and livestock
- Asia: Limited human cases, various livestock species
- Europe: Primarily livestock warbles, rare human cases
- Australia: Sporadic animal cases
Risk Mapping for Travelers
Healthcare providers use epidemiological data to counsel travelers:
High-Risk Destinations:
- Costa Rica and Panama (ecotourism activities)
- Amazon basin countries
- Rural Central America
- Caribbean islands during warm months
Activities Elevating Risk:
- Jungle trekking and camping
- Wildlife observation and photography
- Agricultural or veterinary work
- Extended rural stays
- Adventure sports in natural areas
Prognosis and Long-Term Outcomes
Most botfly infestations resolve completely with appropriate treatment. Understanding expected outcomes helps set realistic expectations.
Typical Recovery Course
Uncomplicated Cases:
- Complete healing within 2-3 weeks after larval removal
- Minimal scarring with proper wound care
- No long-term health effects
- Immunity does not develop; reinfection possible
Complicated Cases:
- Extended healing time with secondary infections
- More significant scarring
- Neurological complications may cause permanent deficits
- Ocular involvement can result in vision loss
Factors Affecting Outcomes
Positive Prognostic Factors:
- Early detection and treatment
- Single larva infestations
- Superficial location
- Healthy immune system
- Proper extraction technique
- Good wound care compliance
Negative Prognostic Factors:
- Delayed treatment
- Multiple larvae
- Deep or aberrant locations
- Immunocompromised status
- Incomplete larval removal
- Poor wound care
Recent Research and Future Directions
Scientific understanding of botflies continues evolving. Current research explores improved prevention and treatment strategies.
Novel Prevention Approaches
Researchers investigate:
- Vaccine development targeting larval proteins
- Biological control using botfly parasitoids
- Pheromone-based trapping systems
- Genetic modification of vector species
- Climate change impacts on distribution patterns
Treatment Innovations
Emerging therapies include:
- Improved pharmacological agents killing larvae more effectively
- Novel extraction techniques minimizing tissue damage
- Better wound healing protocols
- Bioengineered skin substitutes for extensive lesions
Conclusion: Key Takeaways About Botfly Prevention and Treatment
Botfly infestations affect humans and animals across wide geographic areas. While unsettling, these parasitic infections typically resolve completely with proper treatment. Understanding the botfly life cycle, recognizing clinical signs early, and implementing comprehensive prevention strategies provides the best protection.
Essential Action Points:
Travelers: Use insect repellent, wear protective clothing, and inspect your body regularly when visiting endemic areas.
Pet owners: Supervise outdoor activities, use preventive medications during warm months, and check pets frequently for unusual lumps.
Livestock producers: Implement integrated pest management, treat animals appropriately, and monitor herd health systematically.
For everyone: Seek prompt medical or veterinary attention for suspicious lesions. Early treatment prevents complications and ensures complete recovery.
By staying informed and vigilant, you can effectively protect yourself, your family, and your animals from botfly infestations while still enjoying outdoor activities and travel to affected regions.