Introduction
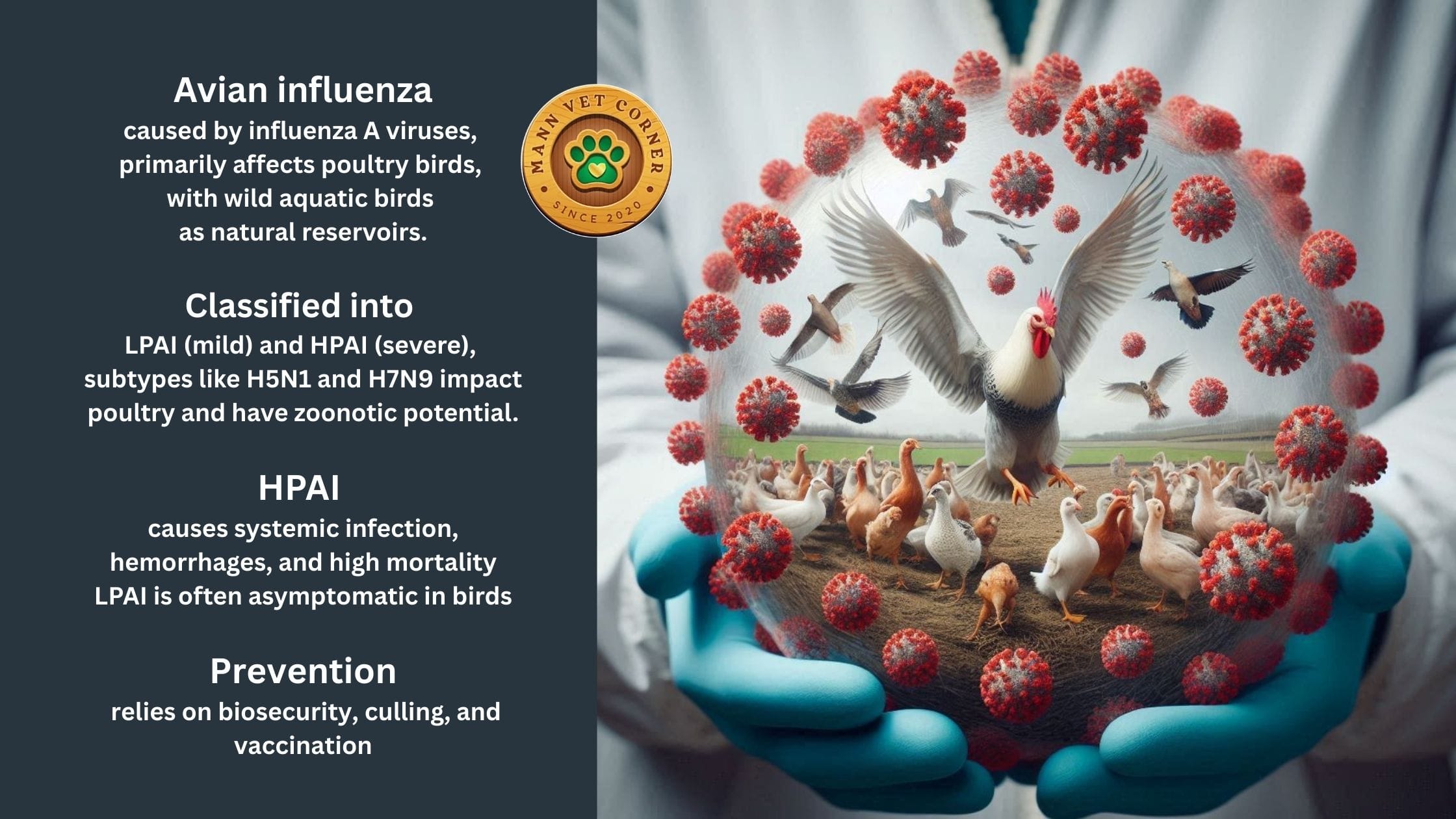
Avian influenza, commonly referred to as bird flu, is a highly contagious viral disease that primarily affects birds, both wild and domestic. It is caused by strains of the influenza A virus and can range from mild to severe forms, with significant economic impacts on poultry industries due to high mortality rates and trade restrictions. While the disease is enzootic in many wild bird populations, outbreaks in domestic flocks can lead to devastating consequences. Understanding avian influenza requires familiarity with key epidemiological terms:
- Endemic: Refers to a disease that is regularly present and stable within a specific geographic area or population, such as low-pathogenic avian influenza viruses circulating continuously among wild aquatic birds without causing noticeable disease.
- Epidemic: Describes a sudden increase in the number of cases of a disease above what is normally expected in a defined community or region, often seen in outbreaks of highly pathogenic avian influenza in poultry farms.
- Pandemic: An epidemic that spreads across multiple countries or continents, affecting a large proportion of the population; in the context of avian influenza, this term is often associated with the potential for zoonotic strains to adapt and cause widespread human infections, as feared with subtypes like H5N1.
This article explores the etiology, classification, history, host susceptibility, transmission, pathogenesis, clinical signs, necropsy findings, mutations, and strategies for prevention and vaccination of avian influenza in birds.
Etiology
Avian influenza is caused by avian influenza A viruses, which belong to the Orthomyxoviridae family. These are enveloped, single-stranded, negative-sense RNA viruses with a segmented genome. The viruses primarily infect birds but have zoonotic potential, occasionally spilling over to mammals, including humans. The etiology centers on the virus’s ability to mutate and reassort, leading to diverse strains that vary in pathogenicity. Wild aquatic birds serve as natural reservoirs, where the viruses often circulate asymptomatically.
Classification of the Virus
Avian influenza viruses are classified based on two surface glycoproteins: hemagglutinin (HA or H), with 16 known subtypes (H1–H16), and neuraminidase (NA or N), with 9 subtypes (N1–N9). This results in numerous possible combinations, such as H5N1 or H7N9. Viruses are further categorized into low-pathogenic avian influenza (LPAI) and highly pathogenic avian influenza (HPAI) based on their genetic features and the severity of disease they cause in domestic chickens. LPAI typically causes mild or no symptoms, while HPAI leads to severe illness and high mortality rates, often exceeding 90% in affected flocks. Pathogenicity is determined by molecular criteria, such as the presence of multiple basic amino acids at the HA cleavage site in HPAI strains.
In poultry birds, not all combinations occur naturally, but certain subtypes are notable for causing outbreaks. The following table summarizes key avian influenza subtypes reported in poultry, classified by HA and NA, along with their typical pathogenicity and examples of impacts:
Short History
The history of avian influenza spans over a century, marked by key discoveries, outbreaks, and evolving global spread. Below is a timeline of significant events:
- 1878: First recorded outbreak in Italy, described as “fowl plague” by veterinarian Edoardo Perroncito, affecting poultry with high mortality.
- 1901-1902: Identified as a filterable agent (virus) distinct from bacteria.
- 1920s: Sporadic outbreaks among birds in Europe and the U.S.
- 1955: Classified as an influenza A virus.
- 1957: Researchers link avian and human influenza viruses.
- 1959: First isolation from wild birds (terns in South Africa).
- 1968: Seasonal flu and bird flu combine, contributing to a human pandemic.
- 1970s-1980s: Multiple LPAI and HPAI outbreaks in U.S. and Europe, including H7N7 in seals (1979).
- 1996: Emergence of HPAI H5N1 in geese in Guangdong, China.
- 1997: H5N1 outbreak in Hong Kong poultry markets; first confirmed human cases (18 infections, 6 deaths); culling of 1.5 million birds.
- 2003-2005: Global spread of H5N1 across Asia, Europe, Africa; becomes endemic in some regions.
- 2013: Emergence of H7N9 in China; causes human epidemics but controlled via vaccination in poultry.
- 2014-2015: H5N2 and H5N8 outbreaks in U.S. and Europe; millions of birds culled.
- 2020-2022: Unprecedented global H5N1 epidemic; affects over 50 million birds in Europe/North America; spills to wild mammals.
- 2023-2025: Continued H5N1 outbreaks; re-emergence in Cambodia (27 human cases since 2023); spread to U.S. dairy cows (over 900 herds in 17 states by 2025); 70 human cases in U.S. since 2024; detections in wild birds and poultry worldwide, with 4,713 animal outbreaks in Americas by early 2025.
Host Susceptibility
Wild aquatic birds, particularly in the orders Anseriformes (ducks, geese, swans) and Charadriiformes (gulls, terns, shorebirds), are the primary natural reservoirs and are often asymptomatically infected with LPAI strains. Domestic poultry, such as chickens, turkeys, and ducks, are highly susceptible, especially to HPAI strains, which can cause rapid and fatal disease. Factors influencing susceptibility include species, age, immune status, and environmental stressors. For instance, gallinaceous birds like chickens are more prone to severe HPAI than waterfowl, which may shed virus without symptoms. Recent changes in epidemiology have seen HPAI becoming endemic in some domestic bird populations and spilling over to wild birds, altering traditional patterns. Mammals, including cats, seals, and humans, can occasionally be infected, but birds remain the main hosts.
Transmission
Transmission occurs primarily through direct contact with infected birds or their secretions, such as saliva, nasal discharges, and feces. The fecal-oral route is common, especially in aquatic environments where viruses can survive in water for extended periods, particularly at low temperatures. Contaminated feed, water, equipment, and fomites facilitate spread on farms. Migratory wild birds play a key role in long-distance dissemination, introducing viruses to new areas. Airborne transmission via aerosols is possible in confined spaces like poultry houses. Vertical transmission (from hen to egg) is rare but documented in some cases. Recent outbreaks highlight the role of wild bird ecology in sustaining and spreading HPAI globally.
Pathogenesis
The pathogenesis of avian influenza in birds begins with the virus entering the host through the respiratory or gastrointestinal tract, where the hemagglutinin (HA) glycoprotein binds to sialic acid receptors on epithelial cells. In low-pathogenic avian influenza (LPAI), the infection is typically localized to the respiratory and intestinal epithelia, leading to mild inflammation and limited viral replication. The HA protein in LPAI strains requires cleavage by trypsin-like proteases, which are restricted to these tissues, resulting in asymptomatic or mild disease with viral shedding primarily through feces.
In contrast, highly pathogenic avian influenza (HPAI) strains possess a multibasic cleavage site in the HA protein, allowing cleavage by ubiquitous furin-like proteases present in multiple tissues. This enables systemic dissemination via viremia, infecting endothelial cells, macrophages, and various organs including the pancreas, spleen, liver, kidneys, heart, lungs, and brain. The virus causes endothelial damage, leading to vascular leakage, hemorrhages, and edema. Necrosis is prominent in affected organs, such as pancreatic acinar cells and splenic lymphoid tissues. A hyperinflammatory response, often termed a cytokine storm, exacerbates tissue damage through excessive production of pro-inflammatory cytokines like TNF-α, IL-6, and IFN-γ, contributing to multi-organ failure and high mortality.
In poultry, particularly chickens, HPAI leads to rapid progression: initial replication in the respiratory tract spreads to the bloodstream within hours, causing widespread apoptosis and necrosis. Neurological involvement may occur due to viral tropism for neurons, resulting in encephalitis. Waterfowl like ducks often exhibit asymptomatic infection despite high viral loads in the intestines, facilitating silent transmission, while gallinaceous birds suffer severe dehydration, cyanosis, and death within 24-48 hours. Recent H5N1 strains (e.g., clade 2.3.4.4b) have shown enhanced neurotropism and adaptation to wild birds, increasing disease severity in previously resistant species. Overall, pathogenesis varies by strain, host species, and immune factors, with high viral replication and immune dysregulation as central mechanisms.
Clinical Signs
Clinical manifestations depend on pathogenicity. LPAI often presents with mild respiratory signs like sneezing, coughing, nasal discharge, and a slight drop in egg production or feed intake, with low mortality. HPAI is dramatic: sudden onset of severe depression, anorexia, cyanosis of combs and wattles, facial edema, diarrhea, neurological signs (torticollis, ataxia), and rapid death within 48 hours. Mortality can approach 100% in susceptible flocks. Waterfowl may show fewer signs but shed high viral loads.
Necropsy Findings
Post-mortem examination of HPAI-affected birds reveals widespread hemorrhages, especially in the skin, muscles, and viscera. Key findings include petechiae on serosal surfaces, necrotic pancreatitis, swollen kidneys with urate deposits, and congested lungs with edema. The trachea may show hemorrhagic tracheitis, and the intestines can be inflamed with mucous exudate. In the brain, meningeal congestion and neuronal necrosis may occur. LPAI lesions are milder, often limited to respiratory tract inflammation and airsacculitis.
Mutations of Avian Influenza: Antigenic Drift and Antigenic Shift
Avian influenza viruses evolve rapidly through two main mechanisms.
>Antigenic drift involves gradual point mutations in the HA and NA genes, leading to minor changes in surface proteins that allow the virus to evade host immunity over time. This is common in endemic settings and contributes to seasonal variations.
>Antigenic shift, a more abrupt process, occurs via genetic reassortment when a host (e.g., a pig or bird) is co-infected with two different strains, swapping genome segments to create novel subtypes. This can result in viruses with pandemic potential, as seen in the emergence of new H5 or H7 strains. Pigs, with receptors for both avian and human viruses, act as “mixing vessels” for shift events.
Prevention and Vaccination
Prevention relies on biosecurity measures: restricting access to farms, disinfecting equipment, controlling wild bird contact, and surveillance through regular testing. In outbreaks, rapid culling of infected flocks, quarantine, and movement restrictions are standard, as per guidelines from the World Organisation for Animal Health (WOAH). Vaccination is used in endemic areas, such as China since 2017 for H7N9 and H5N1, reducing outbreaks significantly. Vaccines are typically inactivated or recombinant, matched to circulating strains, but require updates due to antigenic drift. Global monitoring and early detection are crucial to prevent epidemics from escalating.
In conclusion, avian influenza remains a dynamic threat to avian health and global economies, with ongoing evolution underscoring the need for vigilant surveillance and adaptive strategies.
Frequently Asked Questions
How to prevent and control bird flu in chickens?
Prevention and control involve strict biosecurity practices: restrict access to your property and birds, keep flocks separate from wild birds and wildlife, clean and disinfect equipment, clothes, and hands regularly, and avoid contact with other poultry. Use a color-coded system for hygiene zones on farms. During outbreaks, implement rapid culling, quarantine, and movement bans. Vaccination may be used in endemic areas with inactivated vaccines matched to strains. Surveillance through testing and reporting sick birds early is essential. Keep cats indoors and prevent pets from eating dead birds.
Diagnosis of avian influenza in poultry?
Diagnosis starts with clinical signs (e.g., sudden death, respiratory distress, drop in egg production) and history of exposure. Confirmatory lab tests include virus isolation in eggs or cell culture, real-time PCR on oropharyngeal/cloacal swabs to detect viral RNA, antigen detection via ELISA, and serological tests like agar gel immunodiffusion or hemagglutination inhibition for antibodies. Necropsy reveals characteristic lesions like hemorrhages. Rapid field tests may be used, but confirmation requires WOAH-reference labs.
Pathogenesis of avian influenza in poultry?
In poultry, the virus binds to sialic acid receptors on respiratory/gastrointestinal cells. LPAI remains localized, causing mild inflammation. HPAI spreads systemically via viremia due to HA cleavage site, infecting multiple organs and causing endothelial damage, necrosis (e.g., pancreas, spleen), hemorrhages, cytokine storm, and multi-organ failure. Chickens show rapid death; ducks may be asymptomatic carriers.
How does bird flu spread to humans?
Bird flu spreads to humans primarily through direct contact with infected birds or animals (e.g., poultry, cows), their saliva, mucous, feces, or contaminated environments. This includes handling sick/dead birds, inhaling dust/droplets, or exposure to raw milk/secretions splashing into eyes/nose/mouth. No sustained human-to-human transmission occurs currently, but rare cases from close contact are possible. Risk is higher for farm workers.
What is the difference between bird flu and avian influenza?
There is no difference; “bird flu” is a colloquial term for avian influenza, both referring to the same viral disease caused by influenza A viruses in birds.




Very informative